
(Image by Gerd Altmann from Pixabay)
Throughout my life, I remember hearing about Palliative Care in hushed tones about a Mr. or Ms. So-and-So and their serious cancer diagnosis. The sheer dread and gasp of it. ‘Oh no! they’re on the last train ride to God knows where’ or if I were feeling particularly religious, ‘this poor f*(ked soul is about to meet their maker! And thank God it’s not me!’
WHY ME?
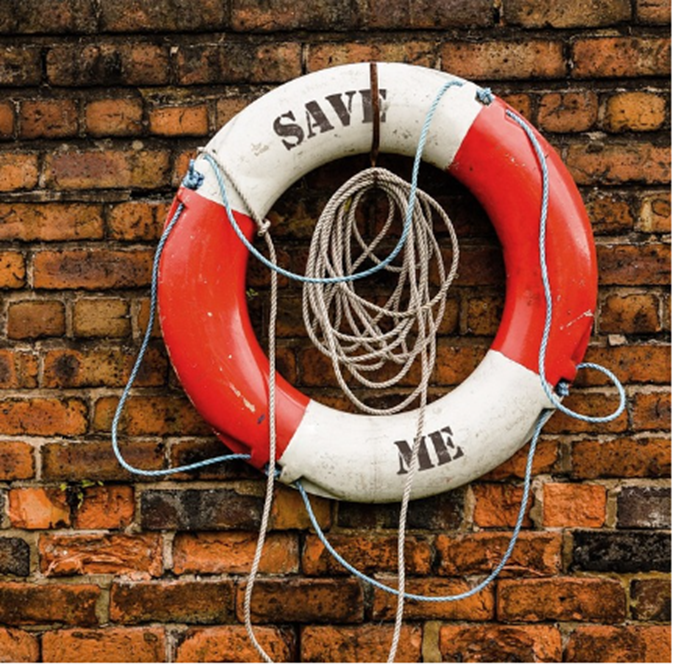
(Image by Shauurk from Pixabay.com)
Three years ago, I began my own Palliative Care journey. I had uncontrollable vomiting which was so bad I lost 23% of my body weight in about six weeks. If I lost 25%, I was told I was at risk of permanent organ damage- or something like that. Not good anyway. So, after 4 cycles of a tough chemo regime, which was successful in reducing my cancer burden, I was put on a milder one. It worked for a while but within six weeks of that I was back to vomiting again and had a rotten distention in my abdomen. Thanks Cancer! So, when the lovely registrar arrived at my hospital bed to declare they were moving me to Palliative Care, I practically jumped and vomited from the fear and shock. Dr. S, took my hand and said, “We are only doing this because they can prescribe stronger drugs than we can. We need to stop your vomiting!” FYI I eventually had surgery – they removed my ovaries, one of which was the size and weight of a baby, and thus the problem resolved. I still have the odd vomit but all very manageable…so far. Touch wood…
STILL PALLIATIVE?

(Pixabay.com)
Upon discharge from hospital, I was told that I would be included in Palliative Care in the community which means that I attend the local hospice. “Hah?!”, as we say in West Cork which is an abbreviation of “What d’ya say?”, “Hah?” adds more shock value. “Hospice? Moi?” I was majorly p!ssed off but too stubborn to let it show so I pretended to be cool and uttered an inaudible “OK, cool. No big deal. Whatever.” Firstly, the nurse called in to see me- I had my own palliative nurse to check if I knew what smorgasbord of drugs and laxatives I were to take and when as well as how I was doing physically, mentally and all the rest. I had a physio check too and guided in regards what exercise I could do post-surgery and for how long and pitfalls to avoid. The highlight of that was if the exercise hurts, rest and stop AKA “Don’t feel the burn!” Then, an occupational therapist visited to see if I needed any modifications to my house, supports, a special bed, a chair for the shower and thankfully I did not need these as my wonderful mother-in-law had these installed prior to her passing. It was like she knew I’d need them too! Not only this but my social worker in the hospital now handed me onto the social worker in the community- and yes, this social worker came from the hospice too. I was allergic now… why would I need a social worker? I am not some orphan! Well, technically I suppose I was and still am, but I was forty-seven! Why would I need a social worker? But then I met her. She explained what areas she would help me with. She said I am here to help you so any finance issues- even in Ireland cancer can be expensive but thank God and Love and Light that we have public healthcare- any problems that may occur, she would help me sort them out including some counselling and how to talk to our son about my diagnosis. I was so thankful to her for helping me in these areas because she also extended her assistance to my husband too. She was there for us as a family, and still is.
PALLIATIVE HAIR, MAKE-UP 'N' SPA

(Image by Angelo Esslinger from Pixabay)
Then my lovely social worker mentioned complimentary therapy. ‘What is that? Some kind of positive thinking where your therapist flatters you to make you feel better?’ Nope. Thanks to fundraising in the community, they can offer me treatments like reflexology and massage after my regular nurse catchups. This depends on the hospice as some hospices are better funded than others. So, some will provide more treatments or activities. In my own one they offer me some natural, handmade lotions and potions for everything from dry skin, muscle ease, menopause, sleep-aid and so forth. Not only this but they offer a service to collect you and drop you at home after your visits. It kinda feels like going to a spa, without the pool facilities or crowds but it is my hospice.
MINGLE, MAKE 'N' DO

(Image by David Clode from Pixabay)
I have to confess something here that I am a little embarrassed about… I was fairly lonely in the beginning of my cancer life. I had moved to a new area- which is lovely- but I knew no one to be honest. The vast majority of my friends were on the other side of the city. One day I found myself crying in front of my ‘palliative nurse in the community’. The next thing I knew she started offering me some activities that I could do in the hospice. There was art and painting, a fatigue course, mince pie making, and Christmas wreath making. Suddenly, I was attending classes with other cancer patients, and I was busy! Initially, it was a bit awkward as I was the youngest patient by far, but we jelled by sharing things we had in common- cancer aches, pains, and side effects- and from there relationships formed. I am still attending my local hospice, three years later.
WHAT DOES PALLIATIVE CARE MEAN?
Not everyone who attends their hospice as a patient dies from their disease but many do. Life is part of death and death is part of life. Isn’t it peculiar how we can spend our entire lives running away from the grief and sadness of death? “Not at all!” I hear you say. And you know what I think you are right in a way. I too spend my days distracting myself from my disease and incumbent death by writing this blog, playing with my son, watching comedies and enjoying what time I have left. Perhaps Marie Kondo has it right. She suggests that to declutter your wardrobe you should hold the item of clothing and ask yourself whether it brings you joy. If it does, then keep it even if you hardly ever wear it. I think I do this with my life on a daily basis. Does this activity bring me joy? If it does, then I do it. Palliative Care is not just for end of life it can also bring quality of life, pain relief and research shows that engaging in it sooner rather than later can extend life. I am doing all that I can do to lengthen mine.
My local specialist hospital has their geriatric doctor as part of the palliative care department and that also changed my view if the term. I took my mother there and while their social services are limited, they are much more available and informal than other hospital departments. It's a vital service and it's great that yours has so much to offer
Thanks nikv! I am so glad you had a good experience with them, and your mum too. Have you ever watched Limitless with Cris Helmsworth ? It has a really good episode on palliative care.
No but I will look out for it
Wonderfully written. I will admit that when I first heard the term Palliative care concerning you it filled me with dread. Now I see that they have so much to offer people in our situation. They are a great support.
P.S. Please accept my apologies for an inconsistent post. For the last 6 to 8 weeks it's been rough. I am out of hospital and hoping to get much better with time and some new drugs, but that's another blog post !
Congratulations @clodaghdowning! You have completed the following achievement on the Hive blockchain And have been rewarded with New badge(s)
Your next target is to reach 3500 upvotes.
You can view your badges on your board and compare yourself to others in the Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPCheck out our last posts: