Arrhythmia substrates in congenital heart disease
In general, arrhythmias in patients with CHD may be due to abnormal anatomy or congenitally displaced or malformed sinus nodes or AV conduction systems, abnormal haemodynamics, primary myocardial disease, hypoxic tissue injury, residual or post-operative sequelae, and genetic influences.2,3 An overview is provided in Figure 1.
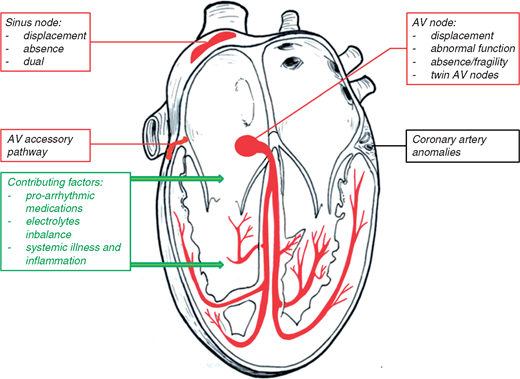
Congenital substrates for arrhythmias in congenital heart defects
Sinus node
Abnormal position of the sinus node may be found not only in rare forms of malformed hearts with juxtaposition of the left atrial appendages but may also be present in patients with sinus venosus defects of superior vena cava (SVC) type. In hearts with left atrial isomerism, sinus node tissue may be completely absent or may be found as remnants in the inferior atrial wall near the AV junction, whereas in right isomerism two sinus nodes may be present.4 An abnormal dysfunctional sinus node can be found in usual position in patients with absence of the right superior caval vein.5
Atrioventricular block
Atrioventricular block in patients with congenitally malformed hearts is most often observed in patients with congenitally corrected transposition of the great arteries (CC-TGA) and in individuals with isomeric arrangement of the atrial appendages, i.e. left isomerism, due to displacement of the specialized conduction system with abnormal development of the central fibrous body.6 The life-long risk of complete AV block in patients with CC-TGA is approximately 2% per year and may reach 50% at 50 years of age.7
Twin atrioventricular nodes
Two distinct AV nodes (‘twin AV nodes’, Mönckeberg sling) may be present in congenital heart defects with AV discordance ([S, L, L] or [I, D, D]) with a malaligned complete AV canal defect and in right and left atrial isomerism giving rise to paroxysmal supraventricular tachycardia (SVT).8
Accessory atrioventricular connections
Accessory AV connections may be present in a variety of patients with CHD with Ebstein’s anomaly of the tricuspid valve being the entity with the highest prevalence. Multiple accessory pathways are often found including special variants with solely anterograde decremental conduction as Mahaim type pathways. Additional types of congenital heart defects with increased prevalence of accessory pathways include heterotaxy syndromes, CC-TGA, AV septal defects, and univentricular hearts.4
Atrioventricular nodal reentrant tachycardia
Atrioventricular nodal reentrant tachycardia (AVNRT) may develop in patients with various types of congenital heart defects at any age. Depending on individual anatomy, localization of the specialized conduction system may be less predictable, particularly in patients with single ventricle (Single V) physiology.9
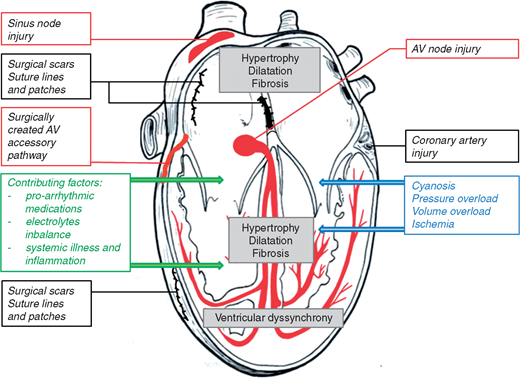
Post-operative substrates for arrhythmias in congenital heart defects
Sinus node dysfunction and atrioventricular block
Direct injury to the sinus node may occur by surgical incisions or suturing in the high right atrium. Atrial switch procedures for patients with d-transposition of the great arteries, Fontan procedures for patients with Single V physiology and rerouting of partial anomalous pulmonary venous return are the most frequent surgical interventions resulting in chronotropic incompetence. More than 50% of survivors from the Mustard operation, for instance, have lost reliable sinus rhythm by adulthood.10 Sinus node dysfunction is often associated with limited exercise capacity and aggravation of AV valve regurgitation which in turn may contribute to development of macroreentrant atrial tachycardia (MRAT).4,10 The conduction system is particularly susceptible to injury during surgical and catheter procedures in patients with ASDs and CC-TGA.10 In addition, perimembranous ventricular septal defect is associated with increased risk for AV block related to percutaneous closure at younger age.
Macroreentrant atrial tachycardias
Macroreentrant atrial tachycardia include incisional intraatrial tachycardias and atrial flutter (AF). Atrial tachycardias (AT) are frequently encountered after surgical repair of a wide variety of congenital heart defects. Incisional atrial arrhythmias may occur even 10 to 15 years post-surgery. Anatomical substrates of reentrant ATs are areas with pre-existing intraatrial conduction abnormalities as well as suture lines, scar tissue, and/or prosthetic material. A stable reentrant circuit may occur around these structures of electrical isolation and anatomic obstacles, such as the orifices of the great veins and the AV annuli, often utilizing a protected zone of atrial tissue with or without slow conduction. Over 60% of these atrial reentrant circuits involve the cavo-tricuspid isthmus (CTI). Scar-related reentrant AT and AF are the most common types of SVT in adult CHD patients. Typical congenital heart defects include atrial septal defects (ASD), tetralogy of Fallot (TOF), Ebstein anomaly of the tricuspid valve, Single V physiology after Fontan procedure, and d-transposition of the great arteries after atrial switch operation1,11 (Figure 2).
Hi! I am a robot. I just upvoted you! I found similar content that readers might be interested in:
https://academic.oup.com/europace/advance-article/doi/10.1093/europace/eux380/4944677