
Hello steemians this is me Anil from Nepal sharing my ideas and information about vaccines and vaccination.

How the vaccines work, the science behind vaccination?
Vaccines are like a training course for the immune system. They prepare the body to fight disease without exposing it to disease symptoms.
When foreign invaders such as bacteria or viruses enter the body, immune cells called lymphocytes respond by producing antibodies, which are protein molecules. These antibodies fight the invader known as an antigen and protect against further infection. According to the Centers for Disease Control and Prevention (CDC), a healthy individual can produce millions of antibodies a day, fighting infection so efficiently that people never even know they were exposed to an antigen.
Unfortunately, the first time the body faces a particular invader, it can take several days to ramp up this antibody response. For really nasty antigens like the measles virus or whooping cough bacteria, a few days is too long. The infection can spread and kill the person before the immune system can fight back.
Vaccines are made from the same germs (or parts of them) that cause disease; for example, polio vaccine is made from polio virus. But the germs in vaccines are either killed or weakened so they won’t make you sick.
Vaccines containing these weakened or killed germs are introduced into your body, usually by injection. Your immune system reacts to the vaccine in a similar way that it would if it were being invaded by the disease — by making antibodies. The antibodies destroy the vaccine germs just as they would the disease germs — like a training exercise. Then they stay in your body, giving you immunity. If you are ever exposed to the real disease, the antibodies are there to protect you.
The science behind vaccination
Vaccines containing these weakened or killed germs are introduced into your body, usually by injection. Your immune system reacts to the vaccine in a similar way that it would if it were being invaded by the disease — by making antibodies. The antibodies destroy the vaccine germs just as they would the disease germs — like a training exercise. Then they stay in your body, giving you immunity. If you are ever exposed to the real disease, the antibodies are there to protect you.

source-http://www.vaccineinformation.org/vaccine-basics/
The pros & cons of a specific vaccine or vaccination in general
The Pros.
- Most medical doctors and other healthcare professionals are positive about what has been achieved through vaccination in preventing and eradication a number of life threatening diseases. The pros are weighty enough to be considered. Here are some:
- Prevention of disease is one of the most important advantages of vaccination. Whether going in disease prone areas or just getting a vaccine during childhood, vaccination has really done much to prevent diseases like polio, whooping cough and various types of fevers.
- Disease eradication. Vaccination programs have been carried out extensively and have totally eradicated life threatening diseases from the human race. It is more than the vaccinated protecting the unvaccinated because here, the threat is done away with completely.
- A lot of money has been saved since the advent and adoption of vaccination. This is money that would have otherwise been used in getting medical attention and buying medication. Other amounts would have been used in developing medicines and research that goes with it.
The cons. - Susceptibility of new born babies in the event mothers have used intravenous diseases. Babies can contract diseases like hepatitis if their mothers have been using such vaccination.
- Artificial immunity will compromise the body’s ability to defend itself for a long time. Natural immunity can last longer. For instance, contracting chicken pox can give you a lifelong immunity against the disease as the antibodies will be aptly developed to defend the body against the real disease.
- There is the risk of harmful and toxic chemicals being introduced to the body. Some people or even children may react severely to these chemicals. The chemicals include.
- Mercury- this is a toxic substance that possess great risks to people. Enough has been said of the dangers of this substance.
- Aluminum- aluminum is a metal that has been associated with dementia, Alzheimer’s disease and seizures.
- SV40- the simian virus 40 is associated with tumors. This is prevalent in children and is traceable to the monkey tissue used in making the polio vaccine.
- Formaldehyde- this is a chemical widely known for causing cancer.
 http://www.researchaustralia.com.au/pros-and-cons-of-vaccination/
http://www.researchaustralia.com.au/pros-and-cons-of-vaccination/
The history of vaaccines, how vaccines have evolved through the years
Evidence exists that the Chinese employed smallpox inoculation (or variolation, as such use of smallpox material was called) as early as 1000 CE. It was practiced in Africa and Turkey as well, before it spread to Europe and the Americas.
Edward Jenner’s innovations, begun with his successful 1796 use of cowpox material to create immunity to smallpox, quickly made the practice widespread. His method underwent medical and technological changes over the next 200 years, and eventually resulted in the eradication of smallpox.
Louis Pasteur’s 1885 rabies vaccine was the next to make an impact on human disease. And then, at the dawn of bacteriology, developments rapidly followed. Antitoxins and vaccines against diphtheria, tetanus, anthrax, cholera, plague, typhoid, tuberculosis, and more were developed through the 1930s.
The middle of the 20th century was an active time for vaccine research and development. Methods for growing viruses in the laboratory led to rapid discoveries and innovations, including the creation of vaccines for polio. Researchers targeted other common childhood diseases such as measles, mumps, and rubella, and vaccines for these diseases reduced the disease burden greatly.
Innovative techniques now drive vaccine research, with recombinant DNA technology and new delivery techniques leading scientists in new directions. Disease targets have expanded, and some vaccine research is beginning to focus on non-infectious conditions such as addiction and allergies.
More than the science behind vaccines, these timelines cover cultural aspects of vaccination as well, from the early harassment of smallpox variolators (see the intimidation of a prominent minister described in the 1721 Boston Smallpox Epidemic entry) to the establishment of vaccination mandates, to the effect of war and social unrest on vaccine-preventable diseases. Edward Jenner, Louis Pasteur, and Maurice Hilleman, pioneers in vaccine development receive particular attention as well.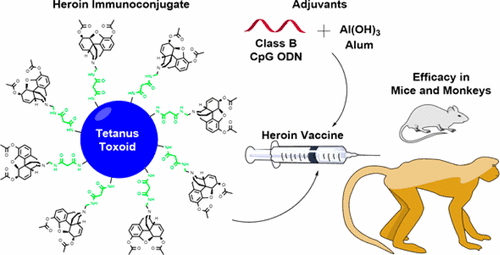
Recent advances in vaccination, new researches regarding it, review of the scientific articles:-
1. Recent advances in Vaccine Development Dr. Mansij Biswas Dr. Pooja Vaidya Dr. Anup Petare Department of Pharmacology & Therapeutics Seth GS Medical College & KEM Hospital2. “A vaccine is a biological preparation that improves immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism, and is often made from weakened or killed forms of the microbe, its toxins or one of its surface proteins. The agent stimulates the body's immune system to recognize the agent as foreign, destroy it, and remember it, so that the immune system can more easily recognize and destroy any of these microorganisms that it later encounters”– WHO 20153. Milestones in vaccine development 1798: Edward Jenner invented smallpox vaccine 1885: Louis Pasteur developed the first vaccine to protect humans against rabies 1927: BCG vaccine recognized 1955: Dr. Jonas Salk’s inactivated polio vaccine licensed, beginning the decline of polio worldwide.4. 1963 : Dr. Albert Sabin introduced trivalent oral polio vaccine The first measles vaccine licensed 1971 : The MMR vaccine licensed. 1982 : Hepatitis B vaccine becomes available. Blumberg & Millman Irwing 1995 : Varicella vaccine is licensed. Hepatitis A vaccine licensed. Acellular pertussis vaccine licensed Milestones in vaccine development5. 2003: The first live attenuated influenza vaccine(FLUMIST) licensed for use in people from 5 to 49 years of age. 2005: FDA licenses the meningococcal conjugate vaccine to prevent invasive meningococcal diseases (MENATRA) 2006: FDA licenses the HPV (GARDASIL) and Rotavirus vaccines (Rota Teq) 2008: Two dose rotavirus vaccine (ROTARIX) approved 2009: Influenza A (H1N1) vaccine approved Milestones in vaccine development6. They help healthy people stay healthy Benefit not only individuals but also communities, and even entire populations (Herd immunity) For most vaccines, their impact on communities and population is more rapid than that of many other health interventions, cost saving as well Reduce prevalence and incidence of diseases, sometimes eradicates the disease itself (small pox, polio) CDC has put vaccination at the top of its list of ten great public health achievements of the 20th century. “With the exception of safe water, no other modality, not even antibiotics, has had such a major effect on mortality reduction”….WHO What is so special about vaccines?7. Concept of vaccination:8. Types of vaccines Whole-Organism Vaccines Killed (Pertussis, Cholera, Rabies, Influenza) Live Attenuated (BCG, OPV, Measles, Mumps, Rubella) Purified Macromolecules as Vaccines Toxoids (Diphtheria, Tetanus) Cellular fractions: • Capsular polysaccharides (pneumococcal) • Cell wall polysaccharides (meningococcal) • Surface antigens (Hepatitis B polypeptide) Combinations (DPT, MMR)9. Newer approaches: Recombinant vaccine DNA vaccine Multivalent Subunit Vaccines According to microorganism I. Bacterial (BCG, Cholera, Typhoid, toxoids) II. Viral (OPV, MMR, Rabies, Hepatitis) III. Rickettsial (Epidemic typhus) According to indication I. Preventive II. Therapeutic 1010. Basic steps of vaccine production11. SELECTING THE STRAINS FOR VACCINE PRODUCTION GROWING THE MICRO- ORGANISMS- PROPAGATION ISOLATION & PURIFICATION INACTIVATION OR ATTENUATION FORMULATION OF VACCINE QUALITY CONTROL AND LOT RELEASE Upstream processing Downstreamprocessing12. Future prospects •Use of recombinant DNA technique to insert the gene coding for the protein of interest into the genome of avirulent virus that can be administered as vaccine •Including in the vaccine only those subviral components needed to stimulate protective antibody, minimizing occurrence of adverse reactions •Use of purified proteins isolated from purified virus or synthesized from cloned genes (recombinant Hep B vaccine containing viral proteins synthesized in yeast cells)- forming empty VLP •Use of synthetic peptides corresponding to antigenic determinants on a viral protein, thus avoiding reversion to virulence since no viral nucleic acid is present (newer HIV vaccines)13. •Development of edible vaccines where transgenic plants synthesizing antigens from pathogenic viruses provide new cost effective way of vaccine delivery •Use of naked DNA vaccines in which recombinant plasmids carrying the gene for the protein of interest are injected into hosts and the DNA produces immunizing protein •Administration of vaccines locally to stimulate antibody at the portal of entry (aerosol vaccines for respiratory disease viruses) •Needle free adminstration: oral (Live Bacterial Vector, Particulate Formulations, Mucosal Adjuvants) transcutaneous, liquid jet injection and epidermal powder immunization, microneedle-based injection system14. Reverse Vaccinology • Conventional approach : Pathogenic organism is grown in the laboratory and from which a limited number of antigens are isolated. • Genes most likely to correspond to conserved antigens are picked out that could be used in a vaccine. • Genes inserted into a different, rapidly multiplying organism – such as yeast •Classical reverse vaccinology: group B meningococcal vaccine.15. Conjugation technology • The sugar molecules linked on the outer envelopes of certain bacteria such as the pneumococcus, the meningococcus, and the Hib bacterium – are Conjugated to strongly immunogenic “carrier” proteins. Old New Protective immunity in children under two years of age. No Yes Create a long-lasting memory of the pathogen No Yes Herd immunity (e.g. Pneumococcus) NO Yes16. DNA Vaccines: a promising future •DNA vaccines are third generation vaccines, and are made up of a small, circular piece of bacterial DNA (called a plasmid) that has been genetically engineered to produce one or two specific proteins (antigens) from a micro-organism. The vaccine DNA is injected into the cells of the body, where the "inner machinery" of the host cells "reads" the DNA and converts it into pathogenic proteins17. Advantages of DNA Vaccines •Cheaper and easier to produce •Large rapid GMP manufacturing capabilities •No need to handle infectious pathogens during production •Safer •Can elicit both humoral & cell mediated immunity •Stable at a broad range of temperature (no cold-chain requirement) •Can be designed and produced by genetic engineering to have only the desired antigens or antigenic sequences (epitopes) in the vaccine •Ability to immunize against multiple antigens and/or Pathogens •Nonviral and no induction of anti-vector immunity18. Vaccine Development Process development Clinical development Assay development Bulk manufacturing Product finishing Phase I Phase II Phase III Purity Potency Stability Discovery19. Nature, 463–469 (26 May 2011); A 2020 vision for vaccines against HIV, tuberculosis and malaria20. 1902: Biologics Control Act/ Virus-Toxin Law 1997: FDA Modernization Act Clinical development Pre-IND Identification of product, component, antigen Manufacturing process Preclinical studies Investigational new drug IND application Clinical studies (Phase I, II and III) Non clinical development studies Licensing Biologics license application Preapproval lot release inspection Bioresearch monitoring Review of label Post approval Lot release testing Biannual or annual facility inspections Post marketing surveillance21. Pre-IND stage Identification of components and antigens Preclinical testing to rule out overt toxicity identify potential toxic effects that might occur during the clinical trial and reversibility of the toxicity Requirements for preclinical toxicity studies depend on, vaccine’s potential risk/benefit consideration target population available clinical data from the use of related products availability of animal models22. Investigational New Drug Stage Phase I Safety & immunogenici ty study Phase II Safety/ Dose ranging study Phase III Large scale safety/efficacy study in small numbers (e.g. 20-100) of healthy adults, apprx 1 year to evaluate vaccine safety and immunogenicity includes study of dose and route of administration Information about the induction of cell-mediated immunity, the cross reactive antibodies and/or interaction pre-existing antibodies which might affect immune system is also obtained.23. Investigational New Drug Stage Phase II Initial trials examining safety, effectiveness (immunogenicity) dose range & pharmacokinetics In several hundred volunteers forming the target groups, like, children, adults or those at risk of exposure to pathogens 1-3 years To obtain preliminary estimates on rates of common adverse events24. Investigational New Drug Stage Phase III provides the critical documentation of the vaccine’s safety and effectiveness needed to, evaluate the risk/benefit relationship to support licensure typically enrol several thousand subjects. 3-5 years • Manufacturing reproducibility is typically addressed by evaluation of lot consistency and ensuring process validation25. Vaccine licensure based on demonstration of safety, immunogenicity, and efficacy based on ability to manufacture product in a consistent manner Biologics license application (BLA) Data derived from nonclinical and clinical studies Description of manufacturing methods Compliance with GMP requirements Documentation of all raw materials used Data establishing stability of the product Samples representative of the product Description of equipment and facility of each location involved in the manufacture26. Lot-Release Testing includes, Sterility, purity: detects the presence of bacterial or fungal contaminants General safety: detects toxicity Identity: verifies that a product induces specific antibodies after vaccination Potency: verifies immunogenicity, antigen content, or chemical composition Tests for removal of process contaminants Pyrogenicity: detects the presence of fever inducing substances Also, constituent materials such as diluents and preservatives must meet standards for sterility Post approval stage27. Extended stability studies • Tropical countries like India • Maintenance of cold chain Lot to lot consistency studies Periodic facility inspections Licensed establishments are inspected at least every 2 years except for those facilities that manufacture influenza vaccines; these establishments are inspected annually28. Post approval stage Post marketing Surveillance Necessary component of vaccine-safety monitoring Done in large populations over longer periods of time Important objectives: to monitor increase in known reactions to identify rare adverse reactions not detected during pre- licensure studies29. 1986: National Childhood Vaccine Injury Act health professionals and vaccine manufacturers to report specific adverse events after the administration of particular vaccines 1990: Vaccine Adverse Event Reporting System (VAERS) established under the joint administration of CDC and FDA to collect reports of suspected adverse events after administration of all US- licensed vaccines FDA and CDC use VAERS data to monitor vaccine safety Adverse event reporting30. Bridging studies in vaccine trials • Done when there is change in vaccine composition with regard to adjuvant, preservative, or a change in manufacturing process, site or scale • Immunogenicity data can easily be used to extrapolate efficacy results when the immune response correlates with vaccine induced immunity • Designed to demonstrate equivalent immunogenicity i.e. exclude a clinically significant difference in the immune response between the population in whom efficacy was shown and the population to whom those efficacy results are extrapolated Fritzell B; ‘Bridging studies’; Dev Biol Stand. 1998;95:181-8.31. Special concerns A small risk of infection with active or live - attenuated micro-organisms Participants in control groups or when subjected to ineffective vaccines run a risk of contracting the disease Risks associated with vaccines produced by recombinant DNA techniques are not completely known Post trial access to the vaccine should be available to the control group. But, children in control arm may cross the age when vaccine is protective. When a trial of HIV preventive vaccine is being conducted, positive serology may result after the vaccination.32. Limitations of Current Vaccines • Single disease prevention • Require Multiple doses • Not 100 % effective • No sustained Protection • Though less, but have adverse reactions • Most are not safe in pregnancy and immunodeficiency • Biological & environmental stability- difficult • Cost effectiveness • Risk of infection with live-attenuated micro-organisms33. Need for development of newer vaccines !! No effective vaccine available for major mortality causing diseases like Malaria, TB and AIDS Need for effective, potent & stable vaccines Minimal/No adverse reactions New Delivery Techniques for better compliance Lower cost Protect against more diseases & sustained protection Emerging and Re-emerging Diseases Era of progressing antibiotic resistance Certain Pandemic Non-Infectious Diseases34. Recent advances35. Menveo (meningitis vaccine) Quadrivalent conjugate vaccine containing the Neisseria meningitidis serogroups A, C, Y and W-135 For active immunization to prevent invasive meningococcal disease in persons 11 to 55 years of age Single 0.5 ml I.M. injection FDA approval was based on demonstration of efficacy in randomized, multicentre, active controlled clinical trial conducted in the 3539 subjects Adverse events: pain at the injection site, headache, myalgia36. Prevnar 13 (Pneumococcal 13 valent Conjugate Vaccine) Conjugate vaccine containing capsular antigens of Streptococcus pneumoniae serotypes, 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, and 23F Indicated for active immunization for the prevention of invasive disease caused by Streptococcus pneumoniae for use in children 6 weeks - 5 years Approval was based on demonstration of non-inferiority compared to U.S. licensed 7-valent pneumococcal conjugate vaccine (PCV 7) in 2 month-old infants Adverse events : injection site reactions, fever, decreased appetite, irritability, sleep issues, diarrhoea, vomiting, rash37. Vaccine schedule: o For Infants and Toddlers: Four-dose series 0.5ml I.M. at 2, 4, 6, and 12-15 months of age o For Unvaccinated Children: 7-11 months of age: 3 doses at 0.5 mL - the first 2 doses at least 4 weeks apart; third dose after the one-year birthday, separated from the second dose by at least 2 months. 12-23 months of age: 2 doses at least 2 months apart at 0.5mL. 24 months - 5 years: 1 dose at 0.5mL. Prevnar 13 (Pneumococcal 13 valent Conjugate Vaccine)38. Menactra (Meningococcal Polysaccharide Diphtheria Toxoid Conjugate Vaccine) Invasive meningococcal disease by Neisseria meningitidis serogroups A, C, Y and W-135 11-55 years 2-10 years 9 months 2004 2007 2011 Safety evaluated in 4 clinical studies in 3700 participants Adverse events: injection-site tenderness and irritability 9 - 23 months: Two doses 0.5 ml each I.M. 3 months apart. 2 - 55 years of age: 0.5 ml single dose I.M.39. Other official recommendations Zostavax, live attenuated vaccine Approved for use in 50 to 59 years of age Based on a multicenter study in 22,000 people, 50-59 yrs, which showed that Zostavax reduced the risk of developing shingles by 70 percent In January 2011, Menveo approved for use in children 2 - 10 years Based on 2 RCT’s (V59P20 & V59P8), Menveo better than innovator polysaccharide vaccine In August 2013, USFDA approved Menveo for use in infants as young as 2 months of age Based on demonstration of immunogenicity in V59P23 trial40. MenHibrix (Conjugate vaccine) For active immunization against invasive disease caused by Neisseria meningitidis serogroups C and Y and Haemophilus influenzae type b in children 6 weeks - 18 months of age Four doses 0.5 ml each I.M. at 2, 4, 6 and 12 months of age. First dose may be given as early as 6 weeks of age and fourth dose as late as 18 months of age Safety demonstrated in 6767 subjects and Immunogenicity demonstrated in 2925 subjects ADR: Injection site pain, irritability, fever and loss of appetite41. Flucelvax (Influenza vaccine) Inactivated trivalent cell-culture-derived vaccine against A (H1N1, H3N2) & B subtypes For active immunization in adults aged 18 years and older Single 0.5 ml I.M. injection The FDA approval of Flucelvax was based on, RCT during the 2007-2008 influenza season in 11400 adults aged 18 - 49 years showed an 83.8% efficacy rate Immunogenicity confirmed in 3 clinical studies in 1353 subjects Adverse events reported: injection site reaction, headache, fatigue42. Fluarix Quadrivalent influenza vaccine First intramuscular Quadrivalent influenza vaccine 3 years of age and older Recommended dose: 3 – 8 years: Two doses 0.5 ml each I.M., at least 4 weeks apart 9 years and older: Single 0.5 ml I.M. Adverse events: injection site pain, headache, fatigue, myalgia FluLaval is another Quadrivalent influenza vaccine approved for use in persons > 3 yrs of age43. Flublok (seasonal influenza vaccine) Trivalent recombinant vaccine For active immunization against influenza subtypes A (H1N1 & H3N2) and type B in adults 18 - 49 years of age. Single 0.5-mL intramuscular injection An RCT in 4,648 healthy adult subjects demonstrated immunogenicity Adverse events noted were injection-site reaction, headache, fatigue, myalgia Received accelerated approval in Oct 2014 for use in persons 50 years of age and older44. Fluzone Quadrivalent influenza vaccine Inactivated Quadrivalent vaccine 6 months of age and older Dose: 6 months to 35 months: 2 doses of 0.25 ml each I.M 4 weeks apart 36 months to 8 years: 2 doses of 0.5 ml each I.M 4 weeks apart 9 years and older: Single I.M 0.5 ml injection Approval based on immunogenicity studies in 1419 children, 6 – 35 months of age and in 2101 children, 3 to 8 years of age Adverse reactions: Injection site reactions, irritability, abnormal crying, myalgia, fever and vomiting45. TRUMENBA (Meningococcal Group B Vaccine) • Approved on October 29, 2014 via accelerated approval • First vaccine licensed in the US to prevent invasive meningococcal disease by Neisseria meningitides serogroup B in individuals 10 - 25 years of age. • Approval was based on demonstration of immune response in 3 randomised trials in 2800 adolescents • Three doses of 0.5 mL each by intramuscular injection at 0, 2 and 6 months • ADR: Pain at injection site, headache, myalgia and fatigue46. Gardasil 9 (Human Papillomavirus 9-valent recombinant Vaccine) Cervical, vulvar, vaginal and anal cancers caused by HPV types 16, 18, 31, 33, 45, 52 and 58 Genital warts caused by HPV types 6 or 11 Girls and women 9 - 26 years of age 0.5-mL intramuscular injection at 0, 2 months, 6 months Added protection against five additional HPV types 31, 33, 45, 52 and 58 RCT in 14,000 females, 16 - 26 yrs showed, 97% effectiveness in preventing cervical, vulvar, vaginal cancers & 78% in preventing anal cancer • Adverse reactions: injection site reactions and headache47. Afluria needle free influenza vaccine Trivalent inactivated influenza vaccine 5 years of age and older Safety & efficacy demonstrated in a RCT conducted in 15,044 subjects Immunogenicity established in an RCT in 832 subjects, 5 to 17 yrs Dose: 5 – 8 yrs: 1 or 2 doses of 0.5 ml each I.M, at least 4 weeks apart 9 yrs and older: Single 0.5 ml dose via needle-free delivery system approved by the FDA ADR: Pain at injection site, headache, myalgia and fatigue48. Fluzone Intradermal Quadrivalent Inactivated Quadrivalent vaccine against subtype A (H1N1 & H3N2) & B virus Approved for use in persons 18 - 64 years of age Single 0.1 mL dose for intradermal injection Approval based on Immunogenicity studies in 2249 participants Adverse reactions: injection-site reactions, headache and myalgia49. Vaccines in pipeline Preventive Therapeutic50. HIV vaccine Urgent global priority An ideal HIV vaccine goal: Sterilizing immunity Realistic goal: to prevent viremia51. HIV vaccine Candidate Vaccine Component First generation Based on envelope proteins especially gp120 Second- generation Live vectors (such as canarypox) or naked DNA coding for different HIV genes Third- generation Regulatory nonstructural proteins eg. Tat (a transactivator of HIV gene expression) and Nef (a multifunctional protein) Majority of these vaccines are in phase I and phase II studies52. HIV vaccine53. HIV vaccine efficacy trial RV144 Tested the “prime-boost” combination of two vaccines: ALVAC HIV vaccine (Prime) AIDSVAX vaccine (Boost) Lowered rate of HIV infection by 31.2 % with maximum protection at 6 – 12 months ALVAC is a recombinant canary pox vector vaccine that express antigens of HIV-1 subtypes B (gp41 )and E (gp 120) AIDSVAX is a bivalent HIV envelope glycoprotein 120 vaccine IgG3 antibodies binding to the V1/V2 region of HIV’s envelope protein correlated with lower infection rates among those who were vaccinated.54. HIV vaccine RV 305 trial • Ongoing Phase IIB trial • To assess safety and tolerability of late boost regimens of AIDSVAX alone, ALVAC alone, or ALVAC/AIDSVAX combination in HIV-uninfected participants from RV 144 • Goal of the secondary boost is to try to extend and increase the immune response seen in RV144 Ongoing Phase I trial To gather more immunogenicity data in 360 new volunteers using R144 regime HIV vaccine RV 306 trial55. tgAAC09 A recombinant adeno-associated virus type 2, HIV-1 subtype C vaccine Does not contain HIV virus Phase I trial in 80 HIV-uninfected healthy volunteers showed that vaccine was safe, well-tolerated, and modestly immunogenic Phase II, Placebo-controlled, Double-blind, Dose-escalation Trial to Evaluate Safety and Immunogenicity is completed in 2012 Trials to evaluate higher doses and boost injections is ongoing in Africa.56. “Our goal is not to completely eradicate the infection - that would be very difficult - but to produce a vaccine that will prevent not infection but disease. I think this is more possible” Luc Montagnier57. Ebola virus disease (EVD) cAd3 Vectored vaccines: Ebola virus glycoprotein is presented in a replication-incompetent chimpanzee adenovirus 3 Phase 1, dose-escalation trial in 20 healthy adults with bivalent form and in 60 healthy adults with the monovalent form is ongoing rVSV Vectored vaccines in which the Ebola virus glycoprotein is presented in a replication-competent vesicular stomatitis virus First phase 1 trial of the rVSV vaccine is slated to begin soon Hong JE, Hong KJ, Choi WY, Lee WJ, Choi YH, Jeong CH, Cho KI. Ebola hemorrhagic Fever and the current state of vaccine development. Osong Public Health Res Perspect. 2014 Dec;5(6):378-8258. Malaria Pre-erythrocytic vaccines: prevent clinical manifestation Erythrocytic vaccines: prevent invasion of RBC by merozoites & speed parasitized RBC clearance Decrease the symptom severity Transmission blocking vaccines: blocks human to human transmission59. Malaria Circumsporozoite protein (CSP) Merozoite surface protein (MSP) Apical membrane antigen 1 (AMA-1) Multiple Antigen Peptide (MAP) Vaccines Effective immunity Currently in preclinical stages Babita Mahajan et al. Multiple Antigen Peptide Vaccines against Plasmodium falciparum Malaria infection and Immunity 2010:70(11):4613‐462460. Malaria RTS,S/AS02A • Pre-erythrocytic subunit vaccine • Fusion of surface CSP antigen with the HBsAg, formulated with the AS02 adjuvant system • Acceptable side-effect profile and immunogenicity confirmed in children 6 weeks of age or older • Phase 3 trial in 15,460 children in two age categories: 6 to 12 weeks of age and 5 to 17 months of age, showed protection against clinical and severe malaria up to 18 months after vaccination. Sacarlal J et al. Long-term safety and efficacy of the RTS,S/AS02A malaria vaccine in Mozambican children. J Infect Dis. 2009 Aug 1;200(3):329-3661. Dengue CYD-TDV Live attenuated tetravalent vaccine Vaccine efficacy of 57%: Phase III study in 10,275 children aged 2 to 14 years in 5 countries in the Asia-Pacific revealed 3 doses given 6 months apart (at 0, 6 and 12 months) First study of the vaccine on Indian adults aged 18-45 years at five sites found: vaccine safe & immunogenic A second Phase III trial: ongoing in 31000 subjects of Latin America Da Costa VG, Marques-Silva AC, Floriano VG, Moreli ML. Safety, immunogenicity and efficacy of a recombinant tetravalent dengue vaccine: a meta-analysis of randomized trials. Vaccine. 2014 Sep 3;32(39):4885-9262. Tuberculosis Nonliving vaccines: purified antigen subunit vaccines and DNA vaccines Live mycobacterial vaccines: attenuated strains or BCG strains Use of viral vectors such as adenovirus or vaccinia virus63. Tuberculosis Boosting BCG with MVA85A Modified Vaccinia Ankara virus expressing antigen 85A Induces higher levels of both antigen specific CD4+ T and CD8+ T cells when used together with BCG Phase I clinical trials showed excellent safety profile A randomised, placebo-controlled phase 2b trial in 2797 infants revealed 17. 3% vaccine efficacy against tuberculosis McShane H, Pathan AA, Sander CR, Goonetilleke NP, Fletcher HA, Hill AV.Boosting BCG with MVA85A: the first candidate subunit vaccine for tub in clinical trials. Tuberculosis (Edinb). 2005 Jan-Mar;85(1-2):47-52 .64. Tuberculosis Boosting BCG with Mtb72F/AS02A Fusion protein derived from Mtb39A & Mtb32A antigens with AS02A adjuvant system Under development for: Prevention of primary TB infection in young children of highly endemic areas As an adjunct to treatment for TB in adolescents & adults. Phase I study in PPD-negative TB-naïve, healthy adults revealed safety and immunogenicity in healthy adults when given in as 0, 1, and 2-month schedule Currently Phase II trial: Healthy PPD-positive volunteers aged 18- 50 years is ongoing Leroux-Roels et al, Evaluation of the Safety and Immunogenicity of Two Antigen Concentrations of the Mtb72F/AS02A Candidate Tuberculosis Vaccine in Purified Protein Derivative-Negative Adults CLINICAL AND VACCINE IMMUNOLOGY, Nov. 2010, p. 1763–177165. Purified Vero cell Rabies vaccine- Next Generation [PVRV NG] No component of human/ animal origin, Very low residual DNA content No risk of contamination with non-conventional transmissible agents. Phase II clinical trial demonstrated comparability of Verorab and PVRV-NG as regards to safety and immunogenicity Phase III in 816 participants aged ≥10 years demonstrated the immunogenic non-inferiority of PVRV-NG compared with Verorab after three doses of postexposure regimen Li R et al, A next-generation, serum-free, highly purified Vero cell rabies vaccine is safe and as immunogenic as the reference vaccine Verorab® when administered according to a post-exposure regimen in healthy children and adults in China. Vaccine. 2013 Dec 5;31(50):5940-7. doi: 10.101666. Cholera Dukoral Shanchol Killed whole cells plus recombinant B subunit Killed whole cells only For persons >= 2 yrs For persons >= 1 yrs 2 doses given 7 – 42 days apart 2 doses given 14 days apart Booster every 2 yrs Booster every 2 -3 yrs Protection for 2 yrs Protection for 3 yrs May 2014: Two complete doses of Shanchol protected individuals by 86 percent during a recent cholera outbreak in Guinea67. Live Oral Cholera Vaccine VA 1.4 National Institute of Cholera & Enteric Diseases, Kolkata Live attenuated single dose oral vaccine developed by isolating a 'Vibrio cholerae O1 El Tor' strain Genetically engineered to produce only the immunogenic B subunit Phase I trial in 87 subjects revealed safety and 67% seroconversion on day 7 after the first dose Phase II trial will be started soon 2main advantages: Single dose confers higher levels of protection No gene that produces the cholera toxin (gene for subunit A) Suman Kanungo et al. Safety and Immunogenicity of a Live Oral Recombinant Cholera Vaccine VA1.4: A Randomized, Placebo Controlled Trial in Healthy Adults in a Cholera Endemic Area in Kolkata, India68. Rotavac rotavirus vaccine India’s first indigenously developed oral Rotavirus Vaccine live attenuated rotavirus strain 116E Phase III clinical trial in 6,799 infants revealed significant reduction in severe rotavirus diarrhoea by 56% during the first year of life, with protection up to 2 yrs Three doses at the ages of 6, 10, and 14 weeks Well tolerated when co-administered with UIP vaccines Approval pending John J, Sarkar R, Muliyil J, Bhandari N, Bhan MK, Kang G. Rotavirus gastroenteritis in India, 2011-2013: revised estimates of disease burden and potential impact of vaccines. Vaccine. 2014 Aug 11;32 Suppl 1:A5-969. Therapeutic Cancer Vaccines In 1891, Dr. William Coley: first attempt to stimulate the immune system for improving a cancer Intratumoral injections of inactivated Streptococcus pyogenes and Serratia marcescens (Coley's Toxin) Allogeneic tumour vaccine Autologous tumour vaccine70. Tumour type Infectious agent Cervical cancer Human papilloma virus Head & neck cancer Human papilloma virus Hepatocellular carcinoma Hepatitis B & C virus Burkitts lymphoma Epstein-Barr virus Post transplant lymphoproliferative disease Epstein-Barr virus Nasopharyngeal carcinoma Epstein-Barr virus Gastric cancer Helicobacter pylori Primary effusion lymphoma Human herpes virus 8 T- cell leukemia Human T-cell leukemia virus 1, 2 Kaposi’s sarcoma Kaposi’s sarcoma-associated herpes virus Infections associated with cancer development71. Ca Prostate: PROVENGE® (Sipuleucel-T) FDA approval on 29 April 2010. Autologous cellular immunotherapy Treatment of asymptomatic or minimally symptomatic metastatic castrate resistant (hormone refractory) prostate cancer. 3 doses at 2-week intervals increased median survival by 4.1 months in phase 3 RCT Each dose contains minimum of 50 million autologous CD54+cells activated with GM-CSF Adverse events reported: chills, fatigue, fever, back pain, nausea, joint ache, and headache Cheever MA, Higano CS, PROVENGE (Sipuleucel-T) in prostate cancer: the first FDA-approved therapeutic cancer vaccine.Clin Cancer Res 2011 Jun 1;17(11):3520-6. doi: 10.1158/1078-0432.CCR-10-3126. Epub 2011 Apr 6.72. Recombinant vaccinia virus expressing PSA Phase 3 PROSPECT trial is ongoing Randomized, placebo-controlled, multi-centre, global 3-arm trial of PROSTVAC in men with asymptomatic or minimally symptomatic, metastatic, castrate-resistant prostate cancer. Ca Prostate: rV-PSA (Prostvac) Ravi A Madan,Philip M Arlen, Mahsa Mohebtash, James W Hodge and James L. Gulley*Prostvac-VF: a vector-based vaccine targeting PSA in prostate cancer Expert Opin Investig Drugs. Jul 2009; 18(7): 1001-1011.doi: 10.1517/1354378090299792873. Breast Cancer: Neuvax (E75) Nonapeptide derived from the extracellular domain of the HER2 protein Two Phase II trials in 195 women with HER-2 positive breast cancer showed a 48% reduction of relative risk of recurrence Phase 3 PRESENT trial (Prevention of Recurrence in Early-Stage Node-Positive Breast Cancer with Low to Intermediate HER2 Expression with NeuVax™ Treatment) is ongoing Two stages of administration: An intradermal injection once per month for six months (6 total) Booster shots once every six months for 30 months (5 total)Milani A, Sangiolo D, Aglietta M, Valabrega G. Recent advances in the development of breast cancer vaccines. Breast Cancer (Dove Med Press). 2014 Oct 14;6:159-6874. Melanoma: POL-103A vaccine Contains multiple melanoma-associated antigens that are shed from 3 human melanoma cell lines Two Phase II trials demonstrated strong efficacy in terms of significantly improved recurrence-free survival and overall survival with excellent safety profile Currently, Phase III MAVIS trial (Melanoma Vaccine in Stage IIb, IIc, and III Melanoma Patients) designed to enrol a total of 1059 patients is ongoing https://clinicaltrials.gov/ct2/show/NCT01546571 accessed on 15.1.1575. Bladder cancer: CG0070 vaccine Type of Oncolytic virus therapy Stimulates cytokine GM-CSF to enhance anti-tumour immune response Phase 1 study with Intravesical CG0070 demonstrated safety and tumour response rate 48 – 77 % Phase 2/3 pivotal BOND (Bladder Oncolytic virus for Non- muscle invasive bladder cancer Disease) trial of intravesical CG0070 for non-muscle invasive bladder cancer patients is ongoing Burke JM et al. A first in human phase 1 study of CG0070, a GM-CSF expressing oncolytic adenovirus, for the treatment of nonmuscle invasive bladder cancer. J Urol. 2012 Dec;188(6):2391-776. Ongoing phase III trials Cancer Vaccine & trial Vaccine type Renal cell cancer AGS-003 (ADAPT trial) DC/APCs Glioblastoma DCVax®-L Rindopepimut (ACT IV) DC/APCs Peptides/proteins Epithelial ovarian cancer Cvac (CANVAS trail) DC/APCs Pancreatic cancer GV1001 (PRIMOVAX) Peptides/proteins NSCLC Stimuvax (START trial) TG4010 Peptides/proteins Virus vectors SCCHN INGN 201 Virus vectors77. Lessons from cancer vaccine trials Cancer vaccines have demonstrated minimal toxicity in all clinical trials with little evidence of autoimmunity Patients who have received less prior chemotherapy are generally more responsive to vaccines Technical and developmental challenges Challenges exist for developing combination therapy that incorporates cancer vaccine with established cancer therapeutics Wolchok JD et al, Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res, 2009 Dec 1;15(23):7412- 20. doi: 10.1158/1078-0432.CCR-09-1624.78. Key factors driving vaccine market in India Relatively low cost of manufacturing Reasonable R & D expenditure Leading edge technology/Combination vaccines Abundant skilled manpower Huge demand High potential for the new vaccines Funding, slow regulatory approval and dependence on government persist as challenges for vaccine development in India79. From global perspective, Rotavirus vaccine Pneumococcol conjugate HPV vaccine From industry’s perspective, Focus is shifting towards DNA and recombinant vaccines To conclude,
@originalworks
To call @OriginalWorks, simply reply to any post with @originalworks or !originalworks in your message!
To nominate this post for the daily RESTEEM contest, upvote this comment!
For more information, Click Here!
!originalworks
Nice to meet you, @anilmehta00! Welcome to the Steemit Community, wish you good luck and a good start, ive send you a small tip and followed you, hope you have an amazing day! :)
thankyou so much @vlone99
This post recieved an upvote from minnowpond. If you would like to recieve upvotes from minnowpond on all your posts, simply FOLLOW @minnowpond
Do not abuse the introduceyourself tag
thanks for participating in the contest. it was a well composed post with lots of informatin..
good luck for the results..
thanks yar