Hello Hivers!
In today's article, I'll explore the epidemiology of Tuberculosis globally and in Nigeria specifically. Tuberculosis (TB) is a potentially serious infection and it affects millions yearly. Let's go.
Pixabay, Photographer: pisauikanImage created by @gamsam. Photo template source:
Introduction
The tubercle bacillus was discovered by Robert Koch in 1882, at a time when the diseases of tuberculosis (TB) was a major killer in Western Europe.
Of minor importance, occurring in West Africa is Mycobacterium Africanum. And rare and of slight importance is Mycobacterium Bovis which causes infection in animals and sometimes in man.
Magnitude of the Tuberculosis Problem
Global distribution:
- 1/3 of world population infected with TB (about 2 billion people)
- About 9 million new TB cases occur annually.
- About 2 million TB deaths occur annually.
- 95% of TB cases occur in developing countries.
- 98% TB deaths also in developing countries.
- Sub Saharan Africa is the worst hit world region by Tuberculosis.
- TB epidemic in Africa is driven by the spread of HIV.
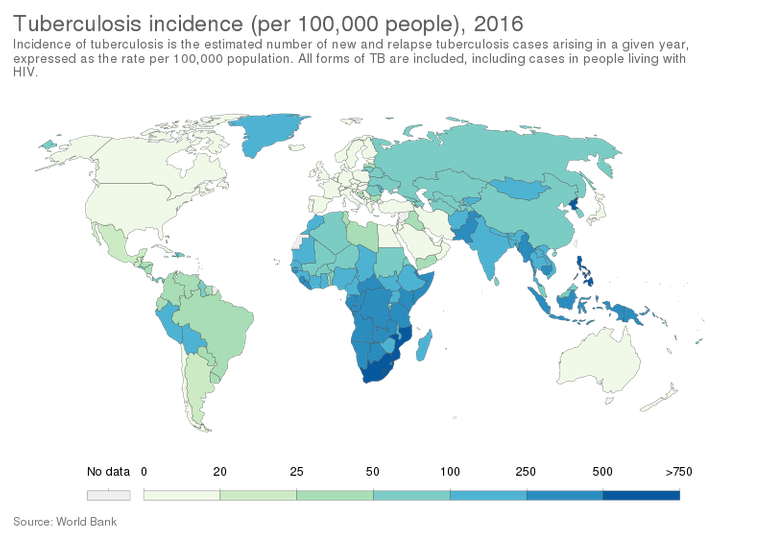
By Our World In Data - https://ourworldindata.org/grapher/incidence-of-tuberculosis-sdgs, CC BY 3.0, Link
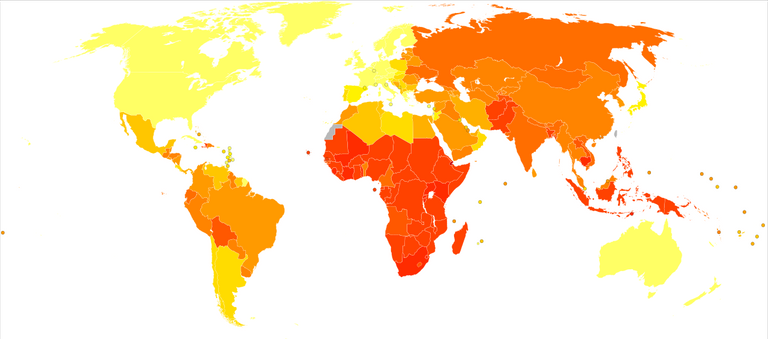
Age-standardized disability-adjusted life years caused by tuberculosis per 100,000 inhabitants in 2004. By Lokal_Profil, CC BY-SA 2.5, Link
In Nigeria:
- About 350,000 cases are estimated to occur annually.
- Nigeria ranks 4th among 22 high burden TB countries in the world.
- Nigeria has the highest TB burden in Africa.
- 50% of these cases are smear positive (most infectious).
- With 4.4% HIV prevalence rate, the country is having a generalized epidemic.
- Case detection rate is only 26% (instead of 70%).
- Economically productive age group (15-50 years) mostly affected.
Epidemiological Determinants
Sources of Infection:
The most common source of infection is the human case whose sputum is positive for tubercle bacilli.
The bovine source of infection is usually infected milk.
Communicability:
The patients are infective as long as they remain untreated.
Effective anti-tuberculosis treatment reduces infectivity by 90% with 48hrs of commencement.
Host factors:
TB affects all ages. However, children, adolescents, the elderly and males are more prone.
TB is not a hereditary disease.
Malnutrition is widely predisposed to infection.
Man has no inherited immunity against TB. Immunity is acquired as a result of natural infection or BCG vaccination.
Social factors:
TB thrives among the lower socio-economic class with poor quality of life, poor housing, overcrowding, population explosion, under-nutrition, illiteracy, poor sanitary conditions etc.
Mode of transmission:
The mode of transmission is mainly be droplet and droplet nuclei generated by sputum positive patients with pulmonary TB.
TB is not transmitted by formites, such as dishes, and other articles used by the patients.
Patients with extra-pulmonary TB or smear-negative TB constitutes a minimal hazard for transmission of infection.
Incubation period:
The time from receipt of infection to development of a positive tuberculin test ranges from 3 – 6 weeks, and thereafter development of disease.
Thus the incubation period depending on host factors and dose of infection may be in weeks, months of years, (usually between 6 – 12 months)
Who is a TB Suspect?
A person is considered a TB suspect if (s)he has some of the following signs and symptoms.
- Cough for 3 weeks or more, with or without sputum
- Coughing up blood
- Unexplained weight loss
- Fever, especially at night
- Chills
- Night sweats
- Loss of appetite
- Tiredness
- Chest pain
- Blood in the sputum
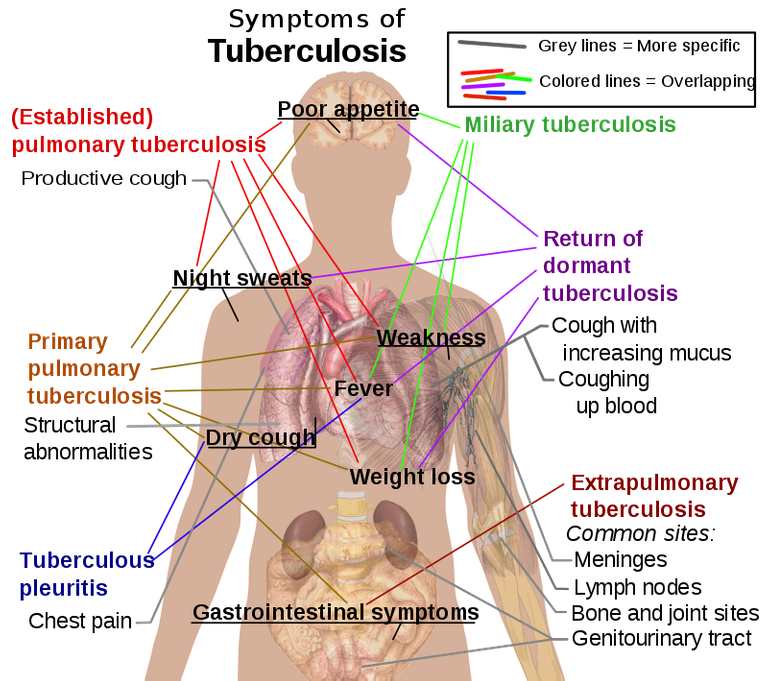
The main symptoms of variants and stages of tuberculosis. By Mikael Häggström. All used images are in public domain., Public Domain, Link
This list is not exhaustive as the signs and symptoms of TB depends on the organ affected and the severity of the disease.
Diagnosis
Diagnosis of tuberculosis by direct sputum microscopy is the method of choice whenever possible. Direct microscopy is relatively cheap, fairly easy to perform and much more specific than chest x-ray.
Recourse to x-rays or other techniques may only be made in the event of repeated smear negativity.
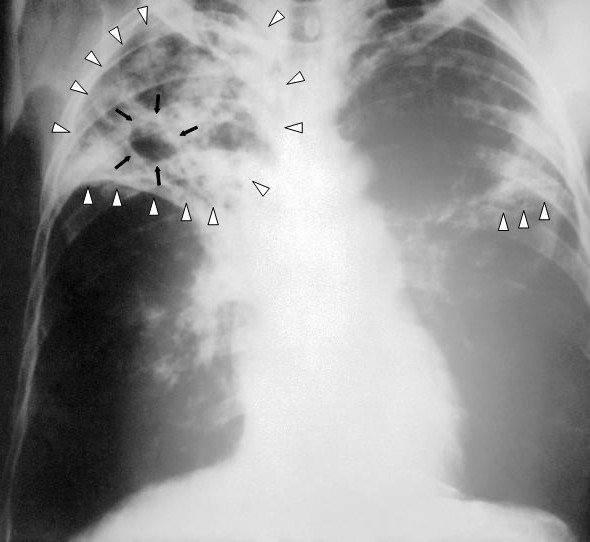
An anteroposterior X-ray of a patient diagnosed with advanced bilateral pulmonary tuberculosis. This AP X-ray of the chest reveals the presence of bilateral pulmonary infiltrate (white triangles), and „caving formation“ (black arrows) present in the right apical region.The diagnosis is far-advanced tuberculosis. By Unknown author - This media comes from the Centers for Disease Control and Prevention's Public Health Image Library (PHIL), with identification number #2543. Public Domain, Link
Other investigations include:
- Tuberculin skin test - a substance called PPD tuberculin is injected just below the skin of your inside forearm. A hard, raised red bump at the injection site after 2-3 days means a likely positive result. This isn't very reliable.

Mantoux tuberculin skin test. By Greg Knobloch - This media comes from the Centers for Disease Control and Prevention's Public Health Image Library (PHIL), with identification number #6806.Public Domain, Link
Blood tests may be used to confirm or rule out latent or active tuberculosis.
Sputum samples can be tested for TB bacteria. Sputum samples can also be used to test for drug-resistant strains of TB.
Classification and Treatment
A TB case is classified broadly into two types: pulmonary and extrapulmonary.
Subsequently, a case is further classified as new or previously treated. The new cases receive and different drug regime from the previously treated.
Key:
Ethambutol - (E)
A combination of Rifampicin and Isoniazid - (RH)
Pyrazinamide - (Z)
Thiacetazone - (T)
Isoniazid - (H)
Streptomycin - (S)
For new cases:
2ERHZ/6TH or 2ERHZ/6EH.
2ERHZ/6EH is usually given to patients who are known to be HIV seropositive or show any signs of hypersensitivity to thiacetazone.
This means that new cases of TB receive 2 months of Ethambutol (E), a combination of Rifampicin and Isoniazid (RH), and Pyrazinamide (Z)
This first phase of treatment is called the intensive phase (2ERHZ) and the intake of drugs is Directly Observed by the health worker or a person trained for the purpose.
Following the intensive phase the new case is placed on the continuation phase (6TH).
During this period the patient collects his drugs, a combination of thiacetazone (T) and isoniazid (H), at the clinic monthly and takes them at home self-administrated for 6 months.
For previously treated patients:
2S3ERHZ/5E3RH3
The total duration of treatment remains unchanged at 8 months. However, the intensive phase last for 3 months instead of 2 months.
Also, an additional drug, streptomycin (S) is included in the drug combination. Note, however, that streptomycin is given for only 2 months (2S), while the other 4 drugs are given for 3 months (3ERHZ)
The Continuation phase here lasts for 5 months as against 6 months for the new cases. Besides, treatment is given 3 times weekly not daily (5E3RH3).
Finally, it is recommended that even this phase be directly observed as this is the patient’s second and last chance to get cured in the control programme.
Potential side effects of TB drugs
- Itching and skin eruptions including Steven-Johnson’s syndrome
- Jaundice/hepatitis
- Joint pains
- Peripheral neuropathy
- Impairment of hearing and balance
- Impairment of vision.
- Pregnant women should not receive streptomycin as this could cross the placental barrier and damage the unborn child’s organ of hearing and balance.
- Similarly, children under 6 years of age should not receive ethambutol. This is because they may not notice or report visual impairments.
- Rifampicin turns the colour of urine orange-red. This is harmless but patients must be informed in advance to avoid undue panic. This phenomenon occurs because the color of the drug rifampicin is orange.

Rifampicin powder. By Thepcmaniac - Own work, CC BY-SA 4.0, Link
The TB/HIV Co-epidemic
The HIV epidemic increases the incidence of TB basically through 2 routes:
- Reactivation of previous (dormant) infection.
- Rapid progression of recently/nearly acquired infection
WHO and NTBLCP discourages routine testing of TB patients for HIV infection. Experience worldwide shows that this practice drives patients underground, worsening both TB and HIV epidemic.
Cost of treatment
All TB and Leprosy drugs and all reagents and materials for diagnosis in Nigeria are provided free of charge by the following organizations.
- German government
- German Leprosy Relief Association (GLRA)
- Damian Foundation of Nederland and
- Sasakawa Foundation of Japan.
The National TB Control Programme
In recognition of the TB problem, the Federal Government of Nigeria established the National Tuberculosis and Leprosy Control Programme (NTBLCP) in 1988 and was formally launched in 1991.
The NTBLCP operates at the 3 tiers of Government. The effort of the Federal Government in the fight against these diseases is being supported by development partners.
Objectives of the TB Control Programme
- To detect/diagnose as many (sputum positive) TB patients as possible, treat them and cure them in order to reduce the number of new cases as well as the level of drugs resistance.
- To treat and cure individual TB patients in order to prevent death.
Targets for TB Control
- To detect at least 70% of the estimated infectious (smear positive) cases.
- To cure at least 85% of those detected.
- MDG: To have halted by 2015 the burden of TB (prevalence and death rates) and reduce it by 50% relative to 1990 levels.
- Global plan: By 2050, the incidence of TB disease will be less than or equal to 1 case per million population per year.
Components of the Stop TB Strategy:
Ensuring high quality DOTS (Directly Observed Therapy, short-course)
- Diagnosis by microscopy
- Political commitment
- Direct observation of treatment
- Un-interrupted drug supply
- Supervision and monitoring
Addressing TB/HIV and MDR-TB
Contributing to health system strengthening
Engaging all care providers, including the private sector.
Empowering people with TB and communities.
Enabling and promoting research.
The control of TB
- Health Promotion
- Specific protection – BCG vaccination for children.
- Preventive therapy – Isoniazide Preventive Therapy (IPT) for contacts.
- Chemotherapy – Mainstay of DOTS (Directly Observed Therapy, short-course)
WHO defines TB control as the achievement of prevalence of the order 1% in the age bracket 0 – 14 years.
Two major components of prevention and control:
- Curative component: namely case-finding and treatment &
- Preventive component: namely BCG vaccination and INH treatment.
The most powerful weapon against TB is the combination of case-finding and treatment.
This is important because it is estimated that an untreated sputum positive TB patient infects 10 – 20 persons every year.
Conclusion
Treatment for tuberculosis is a complicated and lengthy process. But the only way to cure the disease is to stick with your treatment. People with active tuberculosis must take several types of medications for many months to eradicate the infection and prevent development of antibiotic resistance.
Do you have any questions or concerns? Tell me what you think below.
Do you have any questions or concerns? Tell me what you think below.

Resources
- Directly Observed Therapy (DOT) for the Treatment of Tuberculosis - Minnesota Dept. of Health [Internet]. www.health.state.mn.us. Available from: https://www.health.state.mn.us/diseases/tb/lph/dot.html
- Hawn TR, Day TA, Scriba TJ, Hatherill M, Hanekom WA, Evans TG, et al. (December 2014). "Tuberculosis vaccines and prevention of infection". Microbiology and Molecular Biology Reviews.
- Organization, World Health (2008). Implementing the WHO Stop TB Strategy: a handbook for national TB control programmes. Geneva: World Health Organization (WHO). p. 179.
- Wikipedia Contributors. Tuberculosis [Internet]. Wikipedia. Wikimedia Foundation; 2019. Available from: https://en.wikipedia.org/wiki/Tuberculosis
- Tuberculosis - Symptoms and causes [Internet]. Mayo Clinic. 2018. Available from: https://www.mayoclinic.org/diseases-conditions/tuberculosis/symptoms-causes/syc-20351250


All images used are copyright free
Vancouver Style was used for References. Written by @gamsam - a Medical Student
 Robert Koch. By
Robert Koch. By
Good one
Thank you
🙂
Tweet about my post #posh #hive
Tweet
You really pass across a lot of information. I just wish you can make your posts more compact and less webmd-like. Remember, hive is a social blogging platform. You can make it all fun by introducing an element of personality into your writing. Nevertheless, good effort.
Thanks a lot for the tips. I'll make the listed changes.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider supporting our funding proposal, approving our witness (@stem.witness) or delegating to the @stemsocial account (for some ROI).
Thanks for using the STEMsocial app
and including @stemsocial as a beneficiary, which give you stronger support.
A direct microscopy is not end all especially when the result is negative due to low number of bacteria. A culture is required to prove the definitive existence of the bacteria.
Great. Thanks for the addition
Useful content..
Thanks