
CVS makes more than $66 billion bid for Aetna
I woke up today and reviewed the news I had missed this week and I come across another medical industry merger. For those of you not familiar with this sector, allow me to give you a brief summary to this point...
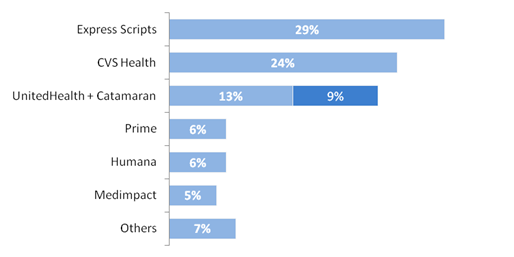
There have been rumors now for some time that Amazon is investigating entering the prescription drug market. This is likely part of what spurred CVS Health, which is comprised of the CVS Caremark pharmacy benefits manager (PBM) and the CVS Pharmacies you can find in most states (the fact that the payer also manages the billing pharmacies is addressed below), to make a bid to acquire Aetna. This would combine the Aetna managed care organization (MCO) with CVS Caremark, the number 2 largest PBM nationally with approximately 25% of the market share(patients). This would not be the first industry example of a PBM and MCO co-existing, though, as United Health created OptumRx as part of their services. Notably, OptumRx recently acquired the Magellan PBM which brings their total market share to around 22% of patients nationally. Are you putting the pieces together now? The industry is consolidating.
Express scripts has already shown interest in creating a partnership with the Anthem MCO, so expect to hear more about this as well. If the CVS-Aetna merger is approved, however, the CVS Health & Aetna conglomerate will have something that the United-Optum group and a potential Express Scripts-Anthem match up would not: Retail Pharmacies. And in this constant battle to stay ahead of the competition, it seems obvious that this would encourage the development of MCO-PBM-Retail Pharmacy juggernauts.
Now why has all of this started in the first place? It seems strange that these massive mergers would be approved by the DOJ given the fact that they have repeatedly blocked MCO mergers over the past several years (see Anthem-Cigna and Aetna-Humana). There is something fundamentally different going on currently though... There has been a heavy focus on PBM transparency from regulators that are concerned with how PBMs pass on rebates and other savings they negotiate from wholesalers and pharmacies, and it has even spilled over into litigation between MCOs and PBMs. Given the current climate, it seems feasible that one could argue better oversight with a direct working relationship under one roof, right?
I for one am concerned about what the continued merging of respective pieces of managed care will do to the healthcare industry. When the Caremark PBM and CVS Pharmacies proposed a merger into CVS Health, I never thought it would be approved by the DOJ. The repercussions would be unfathomable. Yet it was approved and the results have been terrible for the consumer and the small business owner alike. Patients are essentially locked into using only CVS Pharmacies and any independent business that wants to contract with their PBM will be losing money to serve their patients. A similar scenario can certainly develop with the addition of the MCOs.
“I think we have a terrific relationship with Aetna,” says CVS CEO Larry Merlo, “The opportunity is not just in terms of what we can do across our pharmacies, but now you think about infusion in the home, the role of MinuteClinic, now long-term care. I think that there are some exciting opportunities as we think about partnering more broadly.”
Great! Now CVS-Aetna can force their patients to have all of their healthcare provided at minute clinics! This deal would benefit the PBMs and their shareholders, but I struggle to believe the patients are involved in the thought process. They say they are getting more leverage to negotiate rebates, but how much of that will actually passed on to the patients? CVS Caremark netted $177 billion in 2016 which was more than a 15% increase from the prior year, yet Americans continue to shoulder more and more of their healthcare costs, even with the best insurance afforded to them. Copays shifting to coinsurance and deductibles rising rapidly, all because some suits somewhere think that the more "skin in the game" the patient has, the less likely they will be to over-utilize care. In fact, it's more likely patients will avoid treatment altogether because they fear the costs of procedures and medications. And because of the shroud of secrecy that is held over medical billing in this country, they won't truly know what they will pay until the bill is in the mail.
How about a little more competition and lot more transparency?
Congratulations @bru! You have received a personal award!
Click on the badge to view your Board of Honor.
Do not miss the last post from @steemitboard:
SteemitBoard World Cup Contest - Quarter Finals - Day 2
Participate in the SteemitBoard World Cup Contest!
Collect World Cup badges and win free SBD
Support the Gold Sponsors of the contest: @good-karma and @lukestokes
Congratulations @bru! You received a personal award!
You can view your badges on your Steem Board and compare to others on the Steem Ranking
Vote for @Steemitboard as a witness to get one more award and increased upvotes!