In the previous part, we have seen that the chemical imbalance theory is inadequate to explain clinical depression and other mental illnessess. Obseving brain states or neurotransmitter deficinecy or excess cannot provide scientific solutions to the problem of mental illness. Brain states alterations will happen anyway because apparently everything begins and ends in the brain. As emphasized, its not clear whether different brain states are directly correlated with particular symptoms or if the symptoms give rise to particular brain states. There is this fashionable trend from many studies to try to solve the problem of mental illness by finding particular regions and then attribute a causal link. I have seen this idea almost everywhere since the rise of neuroimaging, for example, some psychopaths have a striatum-prefrontal impairment. If you are someone who has spent a few years studying the brain you will probably realize at some point that, well, everything is correlated to everything.
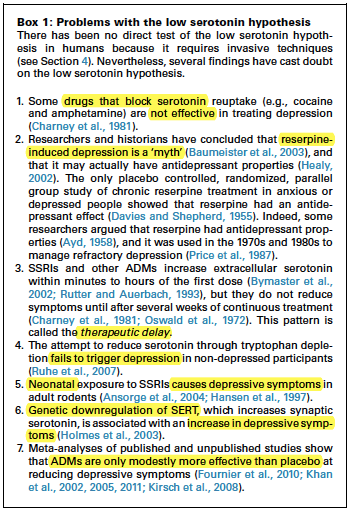
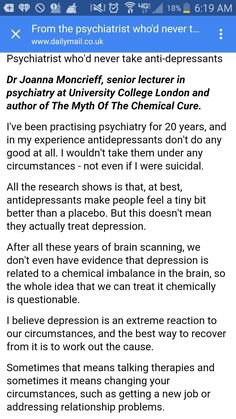
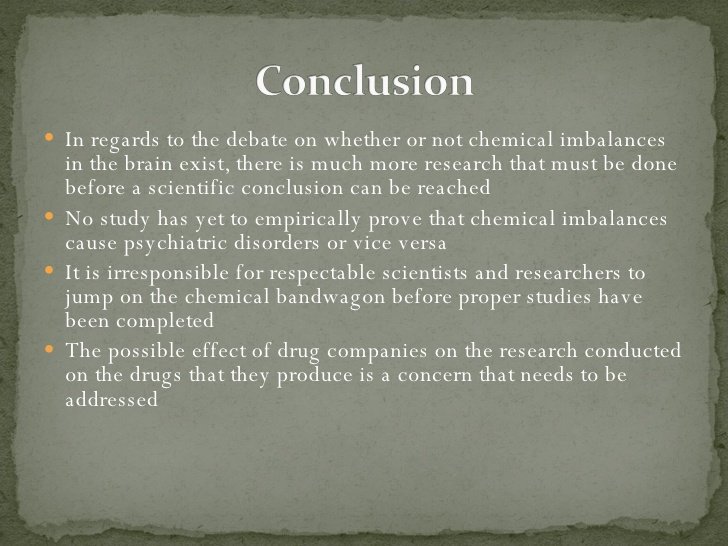
Importantly, the chemical imbalance theory promoted by many psychiatrists with the pressure of the Big Pharma endorses the need of treating the imbalance with pills, in other ways, topping-up your neurotrasmitter levels since they are depleted and this will magically solve the problem. And as I have mentioned, first of all, you need first to specify what chemical 'balance' is before proceeding with the chemical imbalance theory. And even further you will need first to find adequate data that serotonin depletion is the case. And this has not been accomplished for far. Actually, a great deal of research suggests otherwise.
This is not an anti-psychiatry rant or an obsession with political correctness, you know the conservative notion that you can treat everything naturally with vitamins, herbals and minerals, dieting or following some alternative medicine remedies and that using pills is evil. Obviously, in many cases, popping pills is the only way to go. If someone would choose between one treating his wife as a punching bag or some 'bipolar' guy who is about to gamble all his fortune because at the time of his mood peak he feels that he is extremely lucky or some paranoid psychotic woman who wants to stab a police officer because she thinks that she have been tapped all over the place, well, in that case, I would obviously sedate them all. A person who pops a pill to become calmer understands that this is a better approach than letting his outburst take a downward spiral out of control.
However, that's not the case for the majority of the population who chooses to take medication. By accepting the idea that pills can 'balance' the 'imbalance' one becomes ignorant to the dark aspect and the accompanied implications of this. One needs to consider what ELSE happens in the brain apart from the suggested mechanism which in the case of depression is re-uptaking and re-uptaking serotonin, norepinephrine and even blocking dopamine. For instance, for those who are not familar with basic neurobiology, the monoamine doctrine so far is this: a selective serotonin reuptake inhibitor (SSRI) blocks the normal reuptake of serotonin from the synaptic cleft, which is the tiny gap between neurons. Serotonin now stays in the cleft longer than normal and the person begins to feel better.
.jpg)
But so far scientists neglected the fact that all sorts of feedback mechanisms immediately kick into gear now that the brain is shocked. What happens is that the presynaptic neurons begin putting out less serotonin than usual, while the postsynaptic neurons—the neurons receiving the message—decrease the density of their receptors for serotonin.There are changes in beta-adrenergic receptor density and also serotonin autoreceptor activity becomes more sensitive and coupled with serotonin turnover all struggle to compensate from the impact of medication. The same happens when you snort coke every day and built tolerance, to dopamine receptors! Thus, you have, on the one hand the drug which is acting as an accelerator of serotonergic activity but on the other hand the brain responds by putting down the brake!
When messing-around with your chemical soup, the brain and body need to invoke compensatory mechanisms to deal with this neurotransmitter acceleration. An important analysis by the former director of the NIMH makes claims that antidepressants “create perturbations in neurotransmitter functions” causing the body to compensate through a series of adaptations which occur after “chronic administration” leading to brains that function, after a few weeks, in a way that is “qualitatively as well as quantitatively different from the normal state.”
This is also known as “oppositional tolerance'. In essence, this theory says that while on antidepressants, the brain and body try to compensate when they realize that their homeostasis is out of equlibrium and they work in the opposite direction, building tolerance and inducing the very problems they have been originally produced to solve. It usually results in relapse of depression after a prolonged time of continuation and pharmaceutical administration. But what if patients respond well to an antidepressant and then stop taking the drug? Their brains have been modified by exposure to the antidepressant (in other words, an oppositional tolerance has developed), and thus, upon withdrawal of the drug, they are more likely to relapse than if they hadn’t been exposed to an antidepressant in the first place.
Therefore, antidepressants or anxiolytic medication might also be....depressogenic, especially in the long-run. And this is one of the greatest problems that psychiatrists face and where psychiatry becomes a malpractice. It is entirely impossible to predict what a specific drug can do to someone because psychotropic drugs like psychiatric ones are simply not like vaccines or antibiotics or meds that you take for your osteoporosis or Hepatitis, not in terms of their side-effects but in terms of their predictability.
When a doctor sees someone after he has prescribed lexapro he has no idea what he is looking at. If someone was depressed and now he is fine, then one assumes that the drug is actually working. But almost all psychiatric medications (apart from benzodiazpines and anti-psychotics) usually take a few weeks or even a month to kick-in and for an observable, measurable effect to take place. Otherwise, it is impossible to tell a difference between real results and placebos if something begins to work right after you administer it. There are countless cases where a drug makes you even worse before feeling better. Actually, this is a requirement in many cases after administrating a drug.
One needs to feel worse for a few days before improvement. Now, the doctor needs to understand if the worsening of the mood is either because this is what the patient needs to expect in the very first few days or is it because of a side-effect which is usually listed on the label or it could be the case that the patient is having withdrawal symptoms because he has simply forgot to mention or didn't think it was that important to take his meds exactly at 09:00 am than 11:00 am or if the patient is having a sudden relapse after a prolonged time of use or a relapse after quitting the drug and the drug is no longer in his system or of it is a sudden complication from switching meds, coming-down, tirtating and washing-out between meds or if it is due to a bad combo of two or more medications now that monotherapy is virtually non-existent and claimed to be ineffective.
As a guy who has enough experience sitting in a shrink's office for a few sessions and who has a sufficient background in Psychiatry and Neuropsychopharmacology I can safely tell you that, especially in the public sector no doctor will ever go through all the potential variables in a 10-min session.
I don't think that this takes place in any other field of Medicine. And I don't think that this can be even considered as practicing science. And how can you practice science when you are using an obnoxious reductionist 1 condition-1 pill model of human suffering? There is a great chance that prescribed drugs not only do not combat the chemical imbalance but it is more likely creating a chemical imbalance both in the brain and the body. Importantly, the thing is that when it comes to psychiatric medication, its very hard to distinguish between effects and 'side effects' let alone talk about reparative or curative effects.
This is referred to as the drug-based model in Medicine which is observed mostly in Psychiatry. The most applicable analogy is that of the woman with social phobia who finds that drinking two cocktails eases her symptoms. One could imagine, how, this “treatment” could be found efficacious and recommended for daily use and even prevention of symptoms. How her withdrawal symptoms after 10 years of daily use could lead those around her to believe that she “needed” the alcohol to correct an imbalance. This analogy is closer to the truth.
Medicine usually relies on the disease-center model. That drugs should be used to combat an abnormal state like how insulin treatment is used in diabetes. That they work by targeting a specific biochemical imbalance or the very mechanism which produce a natural disease. This does not occur in the case of mental disorders. Most of the time its not about correcting an abnormal state, as the disease model suggests, or working on a particular biochemical mechanism. Psychiatric drugs in their attempt to resolve an imbalance they induce an abnormal or altered state that as a side-effect it suppresses or replaces the manifestations of mental problems. In simple words, psycho-drugs resemble pretty much alcohol and street drugs. They cause altered states of feeling, thinking, and behaving. In particular, they do not treat illnesses. Alcohol, for instance, helps to reduce social anxiety not because it corrects an underlying biochemical imbalance, but because characteristics of alcohol-induced intoxication include relaxation and disinhibition.
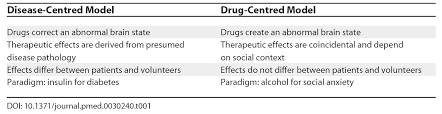
It is the dominant state of intoxication itself that helps, not the effects of the drug on an anxiety mechanism for social anxiety. Or, for instance, opioids target a very specific mechanism by slowing the conduction of messages in the pain nerves but secondary they might produce anti-anxiety features which might be favored by someone who suffers from anxiety. Opioids apparently are not produced or used in medicine to reverse an anxiety mechanism but anxious people might like them because secondary they are producing their own artifical state of relaxation. This is a fact also about 'antidepressants'. Its like using pain killers instead of searching for the source of pain. Some scientists even question why they should be given the label 'anti-depressants'. Psychiatric drugs are like a chemical lottery. Every once and then, they work in the middle of the chemical chaos they produce. Nobody knows how, they just do.
References:
https://www.themedicalsanctuary.com.au/depression-serotonin/
I've read so many bad things about anti-depressants and their side-effects, it's scary. Unfortunately, in my opinion, many shrinks are behaving more like drug-dealers than doctors.
This post has received a 1.04 % upvote from @booster thanks to: @varnavas.