Metastasis and cancer #1
There are about 200 types of cancer known so far (Lambert, Pattabiraman, and Weinberg 2017) and the recent progress in cancer research enabled us to discover common hallmarks, intertwined traits that we hope one day could become a clinical target (Hanahan and Weinberg 2000, 2011). However, there is one trait in particular that stands out: 90% of the deaths caused by cancer occur because of metastasis while only 10% of the deaths are linked to the primary tumor (Lambert, Pattabiraman, and Weinberg 2017).
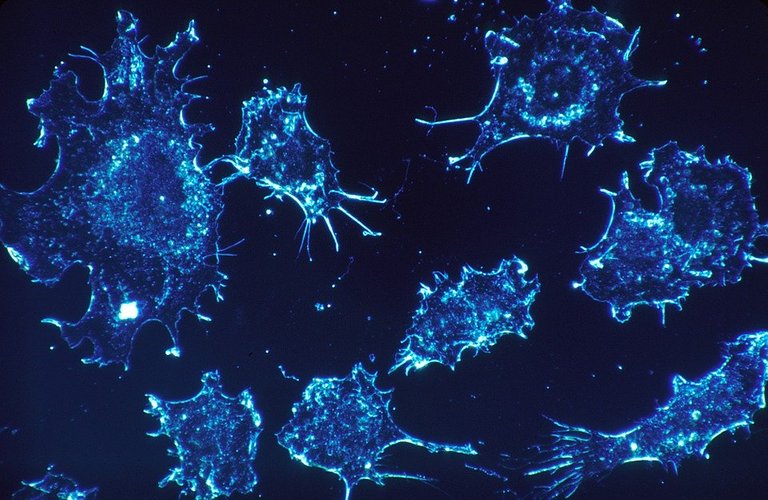
Image CC0 Creative Commons - Source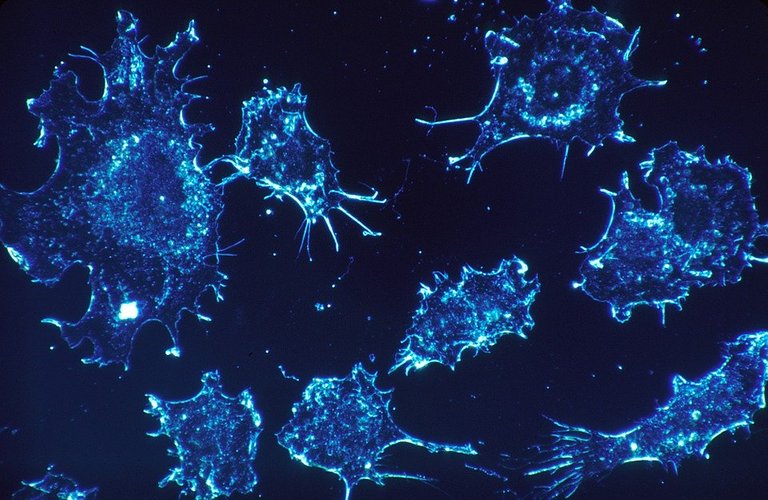
We have a metastasis when cancer cells break away from the original tumor and spread it to a different tissue. Unfortunately, this is a very difficult phenomenon to study and although metastasis cause most of cancer-related deaths, we still know very little about them.
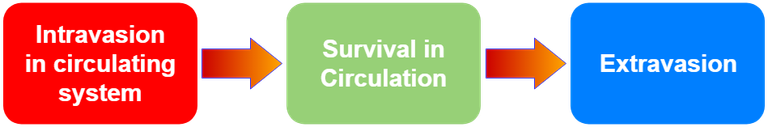
Obviously, I am going to oversimplify, but we can divide the whole process of metastasis in 3 different phases:
- Intravasion of cancer cells in the circulating system
- Survival in circulation
- Extravasion
Image in the public domain - [Source](https://goo.gl/uUh5fN)
We know that generally, cancer exploits physiological mechanisms, often linked to tissue repair, to endow cancer cells with neoplastic properties. For instance, the epithelial/mesenchymal transition (EMT). In this case, carcinoma’s cells lose some of their epithelial phenotype, in favor of a more mesenchymal-like phenotype (Thiery 2002). In other words, carcinoma cells gain the ability to differentiate in different cells types (abnormal differentiation usually results with the acquisition of malignant traits), the ability to degrade the extracellular matrix and overall they become more prone to invade other tissues (Kalluri and Weinberg 2009; Nieto et al. 2016; Thiery 2002). If the EMT programs were more stable they would have been easier to detect, unfortunately there is not a clear transition between epithelial and mesenchymal-like phenotype, thus carcinoma cells show mixed traits.
When there is this phenotype switch the cells are more likely to leave the primary tumor and begin the intravasion process in the circulating system. Now cancer cells enter the most delicate phase, survival in circulation. Although it is estimated that generally circulating cancer cells are in the bloodstream only for a few minutes, they face several obstacles that will most likely be fatal for a large number of them.
Diagram created by the author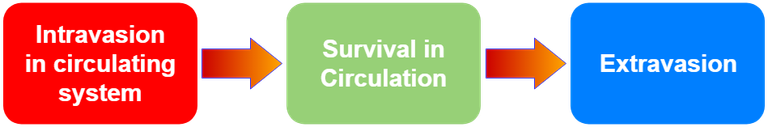
For instance, they will have to be in suspension for a while (most cells prefer to grow on a substrate), face the shear stresses of the bloodstream and most importantly they will likely be exposed to immune cells that could recognize and kill them (Headley et al. 2016). Unfortunately, cancer cells developed several mechanisms to override our defences. First of all, it is very unlikely that a single carcinogenic cell could survive this “journey” (Baccelli et al. 2013), it is more likely that entire clusters of cells, also known as Circulating tumor cells (CTC), are the culprit for the formation of metastasis. Together, cancer cells are more resistant to apoptosis and have higher chances to “lodge” somewhere in the lumen of vessels and begin the third phase, the extravasion (Aceto et al. 2014).
Scientists have tried to exploit the presence of CTC in the bloodstream to develop cancer-detecting kits, it would be wonderful to be able to detect cancer simply by taking a blood sample. Unfortunately, like many things, this sounds too good to be feasible. In fact, the likelihood to detect CTC is extremely small.
In the next post I will discuss about how cancer cells deceive our defences and survive in the bloodstream.
References
Communities that support me are:
enlarge
Attribution-ShareAlike CC BY-SA
Reuse this image by copying and pasting this text with it:
Attribution-ShareAlike CC BY-SA by @elvisxx71 thanks to @aboutcoolscience and @davinci.art
ITASTEM. Click hereIMMAGINE CC0 CREATIVE COMMONS, si ringrazia @mrazura per il logo and vote for @davinci.witness Aceto, Nicola et al. 2014. “Circulating Tumor Cell Clusters Are Oligoclonal Precursors of Breast Cancer Metastasis.” Cell 158(5): 1110–22. http://linkinghub.elsevier.com/retrieve/pii/S0092867414009271.
Baccelli, Irène et al. 2013. “Identification of a Population of Blood Circulating Tumor Cells from Breast Cancer Patients That Initiates Metastasis in a Xenograft Assay.” Nature Biotechnology 31(6): 539–44. http://www.nature.com/articles/nbt.2576.
Hanahan, Douglas, and Robert A Weinberg. 2000. “The Hallmarks of Cancer.” Cell 100(1): 57–70. http://linkinghub.elsevier.com/retrieve/pii/S0092867400816839.
Hanahan, Douglas, and Robert A. Weinberg. 2011. “Hallmarks of Cancer: The Next Generation.” Cell 144(5): 646–74. http://linkinghub.elsevier.com/retrieve/pii/S0092867411001279.
Headley, Mark B. et al. 2016. “Visualization of Immediate Immune Responses to Pioneer Metastatic Cells in the Lung.” Nature 531(7595): 513–17. http://www.nature.com/articles/nature16985.
Kalluri, Raghu, and Robert A. Weinberg. 2009. “The Basics of Epithelial-Mesenchymal Transition.” Journal of Clinical Investigation 119(6): 1420–28. http://www.jci.org/articles/view/39104.
Lambert, Arthur W, Diwakar R Pattabiraman, and Robert A Weinberg. 2017. “Emerging Biological Principles of Metastasis.” Cell 168(4): 670–91. http://www.ncbi.nlm.nih.gov/pubmed/28187288.
Nieto, M. Angela, Ruby Yun-Ju Huang, Rebecca A. Jackson, and Jean Paul Thiery. 2016. “EMT: 2016.” Cell 166(1): 21–45. http://linkinghub.elsevier.com/retrieve/pii/S0092867416307966.
Thiery, Jean Paul. 2002. “Epithelial–mesenchymal Transitions in Tumour Progression.” Nature Reviews Cancer 2(6): 442–54. http://www.nature.com/doifinder/10.1038/nrc822.
Aceto, Nicola et al. 2014. “Circulating Tumor Cell Clusters Are Oligoclonal Precursors of Breast Cancer Metastasis.” Cell 158(5): 1110–22. http://linkinghub.elsevier.com/retrieve/pii/S0092867414009271.
Baccelli, Irène et al. 2013. “Identification of a Population of Blood Circulating Tumor Cells from Breast Cancer Patients That Initiates Metastasis in a Xenograft Assay.” Nature Biotechnology 31(6): 539–44. http://www.nature.com/articles/nbt.2576.
Hanahan, Douglas, and Robert A Weinberg. 2000. “The Hallmarks of Cancer.” Cell 100(1): 57–70. http://linkinghub.elsevier.com/retrieve/pii/S0092867400816839.
Hanahan, Douglas, and Robert A. Weinberg. 2011. “Hallmarks of Cancer: The Next Generation.” Cell 144(5): 646–74. http://linkinghub.elsevier.com/retrieve/pii/S0092867411001279.
Headley, Mark B. et al. 2016. “Visualization of Immediate Immune Responses to Pioneer Metastatic Cells in the Lung.” Nature 531(7595): 513–17. http://www.nature.com/articles/nature16985.
Kalluri, Raghu, and Robert A. Weinberg. 2009. “The Basics of Epithelial-Mesenchymal Transition.” Journal of Clinical Investigation 119(6): 1420–28. http://www.jci.org/articles/view/39104.
Lambert, Arthur W, Diwakar R Pattabiraman, and Robert A Weinberg. 2017. “Emerging Biological Principles of Metastasis.” Cell 168(4): 670–91. http://www.ncbi.nlm.nih.gov/pubmed/28187288.
Nieto, M. Angela, Ruby Yun-Ju Huang, Rebecca A. Jackson, and Jean Paul Thiery. 2016. “EMT: 2016.” Cell 166(1): 21–45. http://linkinghub.elsevier.com/retrieve/pii/S0092867416307966.
Thiery, Jean Paul. 2002. “Epithelial–mesenchymal Transitions in Tumour Progression.” Nature Reviews Cancer 2(6): 442–54. http://www.nature.com/doifinder/10.1038/nrc822.


I remember having read (from @tking77798) that circulating tumors leave DNA tracks so that they can in principle be detected. I was really interested when I read that for the first time, and I am looking forward to read updates about that. Will you mention it as well?
Thank you for your comment, I will have a look at his post. Technically it's possible to detect DNA from cancer cells in the bloodstream, but it's just very challenging because DNA in the blood has a short half-life and cancer cells travel in the bloodstream only for a few minutes but as you know in science things can evolve quickly ;)
Yeah, I naively think this is somehow a way for the future to be mostly already here ;)
Regards, @aboutcoolscience. Interesting your post about cancer. Since metastases are responsible for 90% of deaths from cancer, as explained in the post, it is a pity that the chances of detecting CTC in the blood are very small, otherwise it would be a good starting point to avoid metastasis.
Good read, it's difficult to imagine what might help detect metastasis if detecting ctcs from blood is as hard as you say. Maybe we can find a way to profile cells where ctcs may be likely to form.
I find this subject especially interesting, for personal and family reasons.
I will be waiting for the next part, eagerly.
Thank you for your comment, unfortunately this is a delicate topic for me too for family reasons..do you prefer short and concise posts or would you rather see a longer and more detailed post?
The longer, the more detailed, the better. Thank you.
Very important and informative articles about cancer. Thank you so much for sharing this article