What is Parkinson's Disease?
Parkinson’s disease (PD) is a neurodegenerative disorder with unknown causes. However, it is suspected that to a certain degree its cause might be genetic or environmental. Most of patients are diagnosed in their 60’s; although; early-onset PD does occur (Heyn & Davis, 2018). It has also been recorded that men are much more likely to develop this illness than women are (MayoClinic, 2015). It is the second most common neurodegenerative illness with prevalence as much as 550 cases in 100,000 people and it affects the central nervous system (Valcarenghi et al., 2018). What occurs in patients with PD is that brain cells that produce dopamine degrade and eventually their numbers are lost, thus, resulting in worsening of motor functions (Heyn & Davis, 2018). Valcarenghi et al. (2018) describe it in more detail, stating that it is “characterized by the reduction of nigrostriatal and cortical dopaminergic influence”. Therefore, a patient’s movement, speech and writing may be affected. The symptoms of this illness are primary and secondary.
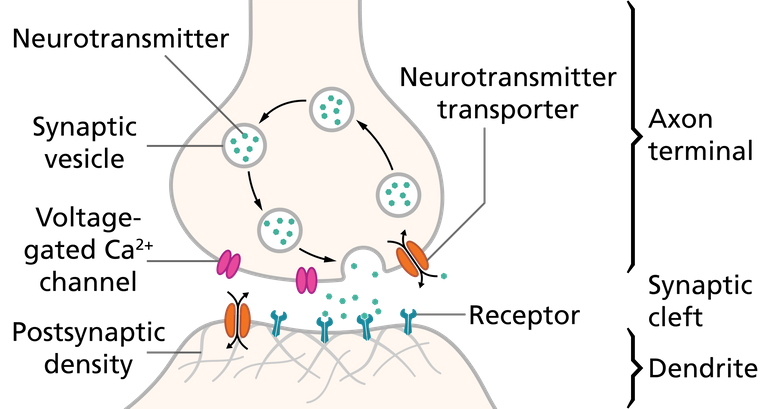
Image Source: Wikimedia Commons, Uploader: Thomas Splettstoesser, License: CC BY-SA 4.0
What are the Symptoms of PD?
The primary symptoms are the main symptoms that characterize the illness itself. In PD these are tremor, stiffness, slowness, balance and posture impairment, shuffling gait, speech and writing changes (Heyn & Davis, 2018; Mayo Clinic, 2015). These signs might make it difficult to complete everyday tasks, such as eating, walking, doing chores or working. Also, the symptoms may become progressively worse. For example, the very first warning signs may be inability to make facial expressions or not swinging one’s arms when they walk (MayoClinic, 2015). These then may grow into a worse symptom. The secondary symptoms are the ones that may appear as a result of primary symptoms. These are signs such as anxiety, depression and dementia (Heyn & Davis, 2018). Valcarenghi et al. (2018) have also discovered that there is a strong correlation between PD and developing depression. This is so, because for people with PD every day may feel like a fight for their independence or on the contrary, loss of their integral self. Patients suffering from PD often report that every day is different and there may be improvements or worsening of their symptoms (Valcarenghi et al., 2018). The primary symptoms are not the only aspects of the illness that patients use medication for. They state that they need to take many different medicines in order to help lower symptoms of other diseases connected with PD that are a result of secondary symptoms, such as anxiety or depression.
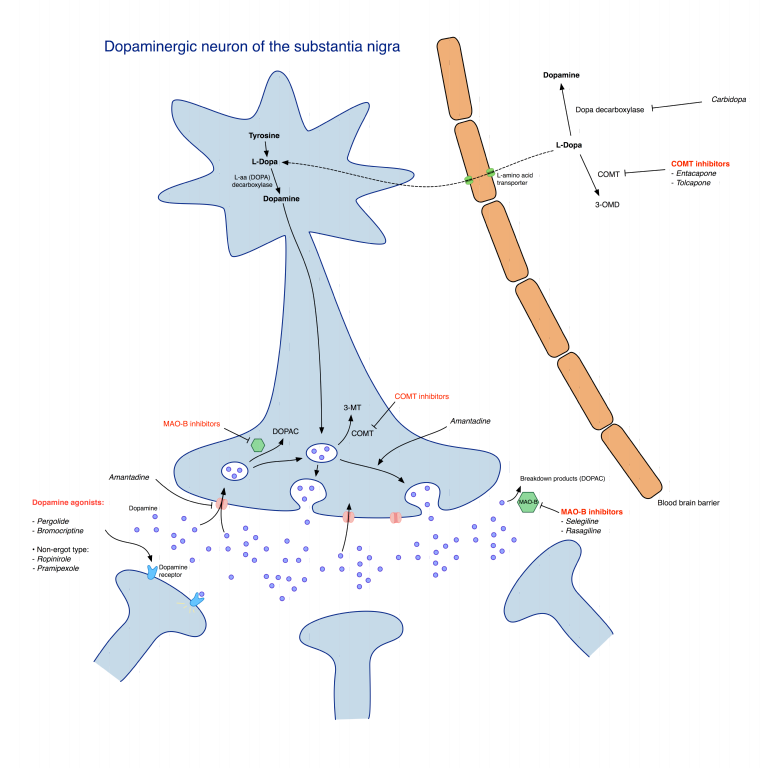
Image Source: Wikimedia Commons, Uploader: Luigi Albert Maria, License: CC BY-SA 3.0
What Might Cause PD?
As was stated earlier, the causes for PD are not known. However, MayoClinic (2015) reports that one’s genes may be one of the causes, especially if this disease runs in families. However, even in cases where PD runs in families, the risk for developing this illness is very small. There are certain gene mutations that may produce this illness, although, this cause is rather rare. Exposure to certain environmental factors or toxins (i.e. herbicides or pesticides) can also result in developing PD later in life; although, this cause is also rare (MayoClinic, 2015). However, it should be noted that changes in the brain occur not only before the development of PD, but also after. One of such changes may be the presence of Lewy bodies which are clumps of particular substances in the brain that are also microscopic markers of PD (MayoClinic, 2015). It is believed that it is important to study these bodies as they might be one of the clues behind what causes this illness. Another article that might appear post-PD is the alpha-synuclein which can be found within Lewy bodies. This protein is found in all Lewy bodies in a clumped form that cannot break down and is thus a great focus of studies (MayoClinic, 2015). Researchers believe that these two clues are the steps that may uncover possible causes of PD. Hence, this is why these hints are subjects of many studies.
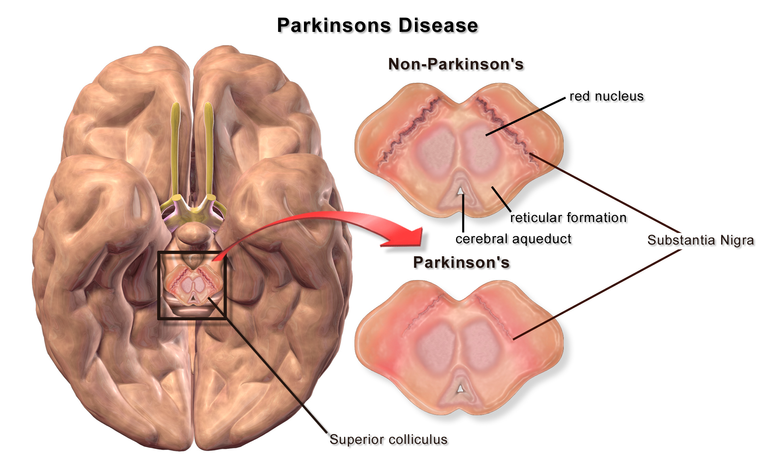
Image Source: Wikimedia Commons ,Uploader: BruceBlaus, License: CC BY 3.0
Medication
While PD is incurable, there is medication that can help lessen the symptoms of this illness. Valcarenghi et al. (2018) have found that one of the drugs that is often administered to patients is Levodopa, with as many as 58% of users reporting side effects. They could be varying from sleepiness to experiencing pain. However, Levodopa is not the only medication of choice. There are also such options such as carbidopa – which works best when taken with Levodopa – dopamine agonists, Amantadine, trihexyphenidyl, benztropine, selegiline, rasagiline, tolcapone and entacapone (Lava, 2017). Some of these medications work better than others, however, there are some that should be taken together (i.e., Levodopa and carbidopa). Dopamine agonists such as ropinirole, pramipexole and rotigotine can be used on their own or along with another drug. Oftentimes, they are the preferred drug to administer to patients. This is because they serve as dopamine, which people with PD need, and do not pose a threat to developing long-term issues like Levodopa does (Lava, 2017). While dopamine agonists are not as effective as Levodopa, they last longer, however, they do not come risk-free (MedicalNewsToday, 2016). The side effects of using this type of medication include development of compulsive behaviour or hypersexuality. Amantadine raises the level of dopamine in one’s brain which helps cope with some symptoms and trihexyphenidyl along with benztropine help restore balance between dopamine and acetylcholine (Lava, 2017). However, because the latter two can negatively impact thinking and memory, they are not prescribed often. Selegiline and rasagiline block certain chemicals that break down dopamine, hence, allowing patients with PD have more of this hormone in their brain (Lava, 2017). These drugs may be found especially useful for those who have developed PD early as it slows down the development of this condition. However, these drugs have their side effects that range from dizziness to pain and development of depression. Lastly, tolcapone and entacapone are best taken with Levodopa, because they block a chemical in one’s body called COMT. This chemical makes certain aspects of Levodopa useless, therefore, tolcapone and entacapone can be used to prevent COMT from harming the process of treatment using Levodopa.

Image Source: Flickr, Uploader: Jinx McCombs, License: CC BY-ND 2.0
Other Therapies
Medications are not the only ways to help people cope with PD. There are various therapies available to help lessen the symptoms. Medical News Today (2016) list such options as exercise, speech, occupational, and physical therapies. Exercise and physical therapy are best performed under the supervision of a qualified physiotherapist. They can help patients improve their mobility, muscle tone and range of motion. Exercise and physical therapy are also beneficial for lessening joint pain and relieving stiffness. This type of treatment combines stretching, using the treadmill, cycling and resistance training (MedicalNewsToday. 2016). Speech therapy focuses on improving a patient’s slurred speech and even swallowing difficulties and use of body language. While occupational therapy helps patients cope with completing simple tasks such as getting dressed or going to the store. These types of therapies can be taken simultaneously and along with medication, they make an excellent way to take care of oneself. While drugs may help patients feel better physically, therapies may improve mental well-being as well as physical.

Image Source: Pixabay, Uploader: sasint, License: CC0 Creative Commons
Surgery
Finally, there is an option of surgery. One of such types of treatment is deep brain stimulation, which is exactly what it sounds like. The procedure involves planting an electrode inside the part of the brain that is responsible for movement while a neurostimulator is placed under the skin in the upper chest area (MedicalNewsToday, 2016). A wire connects these two points and transmits electrical impulses that are sent from the neurostimulator into the brain. This helps block electrical signals that cause PD symptoms. However, there is risk of infection and brain haemorrhage and is only advised to patients who are suffering of a severe stage of PD and does not respond well to medications. Thalamotomy, pallidotomy and subthalamotomy are surgical procedures that involve removing parts of the brain (thalamus, gobus pallidus and subthalamus, respectively) (MedicalNewsToday, 2016). However, while these procedures may lead to improvement of certain symptoms, they are rarely done. If they are completed, then it is mainly used to treat patients who do not respond well or at all to medication.
Conclusion
Because there is no known cause behind PD, there is no advice that can be given to prevent its development. However, it has been noticed that diet and exercise can lower one’s risk of developing the disease.
References
Heyn, S., Davis, C. (2018). Parkinson’s Disease Symptoms, Signs, Causes, Stages, and Treatment. MedicineNet.com. Retrieved from https://www.medicinenet.com/parkinsons_disease/article.htm
Lava, N. (2017). Medications for Parkinson’s Disease. WebMD. Retrieve from https://www.webmd.com/parkinsons-disease/guide/drug-treatments#1
MayoClinic. (2015). Parkinson’s Disease. MayoClinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/symptoms-causes/syc-20376055
MedicalNewsToday. (2016). What Are the Treatment Options for Parkinson’s Disease? MedicalNewsToday. Retrieved from https://www.medicalnewstoday.com/info/parkinsons-disease/treatment-for-parkinsons-disease.php
Valcarenghi, R., Alvarez, A., Santos, S., Siewert, J., Nunes, S., Tomasi, A. (2018). The Daily Lives of People With Parkinson’s Disease. Revista Brasileira de Enfermagem, 71(2).