Hello everyone... especially the scientific community @steemstem, for this occasion I want to share with you a subject that represents a medical urgency and that its diagnosis and rapid treatment means the salvation of the affected member, even the life of the patient.
A compartment syndrome arises as a result of a loss of balance between volume and pressure within a myofascial compartment, leading to decreased blood flow and thus ischemia and tissue death if left untreated.
At the beginning of history, when this pathological entity was described in the first texts, as a picture of Volkmann's muscle contracture resulting from vascular insufficiency in the forearm.
The identification of a compartment syndrome is often a challenge, and we can confuse and attribute the signs and symptoms manifested by the patient to an underlying entity, such as a fracture.
Causes
Regardless of the etiology of the syndrome, the final result will be prolonged vascular ischemia (compression), inflammation (volume overload state or fracture) or the presence of a thrombus in a vessel that irrigates the affected compartment.

Public domain CC BY-SA 4.0
Signs and Symptoms
The most distinctive symptom is the persistent pain, without aching, of strong intensity and that increases with the mobilization, and independent of the cause that originated it.
Increase in volume and changes in local colouring is characteristic.
Decrease or absence of pulses in this area accompanied by coldness of the limb.
Paralysis of the affected muscle group.
Presence of blisters, necrosis by prolonged ischemia, already in late phase.
It is most frequently located in the leg, forearm and buttock.
Waiting for the appearance of all these symptoms is a risk, as it implies the presence of a large group of permanent and dangerous sequels including muscular necrosis and even the possible loss of the limb. A very useful tool in these cases is the measurement of the tissue pressure of the affected muscle compartment, being the most common for the diagnosis of this syndrome in conjunction with the signs and symptoms.
Anatomy
It is described based on the affected area, which involves a muscle group closed in a space by the fascia, the skin or any external force (such as a cast or immobilization) in a site with high potential to develop a compartment syndrome.
Lower extremity: Leg
This zone consists of four well-defined muscle compartments; anterior, lateral, posterior, deep and superficial.
The anterior compartment is made up of the 4 extensor muscles of the leg, whose function is the dorsiflexion of the foot, also through it run the deep peroneal nerve and anterior tibial artery.
Lateral compartment, consisting of long and short peroneal muscles, its function is the eversion of the foot, with abduction and associated plantar flexion. It is irrigated by the superficial peroneal nerve.
The posterior compartment is divided by a fascia layer, which separates them into superficial and deep posterior.
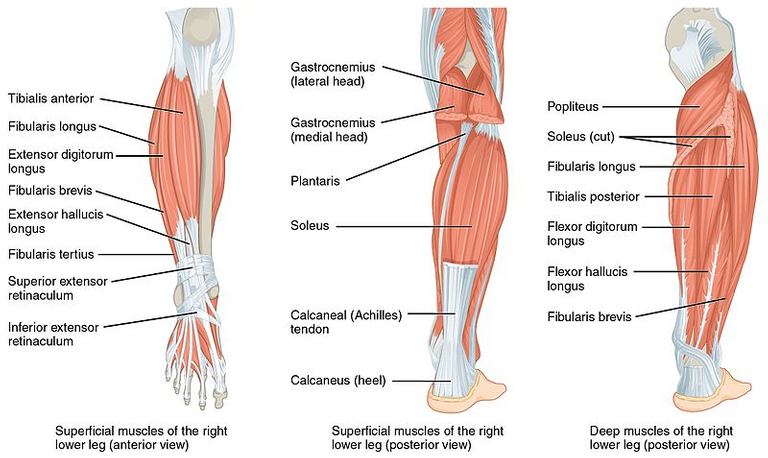
Muscles of the Leg. Public domain Wikipedia CC BY-SA 4.0
The superficial compartment, constituted by the tendons of the twins, soleus and thin plantar. In relation to the deep posterior it contains 4 deep flexor muscles called, long common flexor, long flexor of the first finger, posterior tibia and popliteal, between which runs the tibial nerve, the posterior tibial artery.
These being the most affected areas developed below.
Upper Extremity: Forearm
Consisting of 3 compartments, which are interconnected at various levels, which facilitates that during the decompression of a compartment will also decrease the pressure of adjacent compartments.
For the forearm, the compartments in the volar, dorsal and mobile muscle pad have been fractionated. The volar compartment contains all the flexor muscles of the forearm and hand, as well as the median and ulnar nerves, the radial, ulnar and common interosseous arteries.
The dorsal compartment consists of the extensor muscles of the forearm and hand, as well as the artery and interosseous nerve.
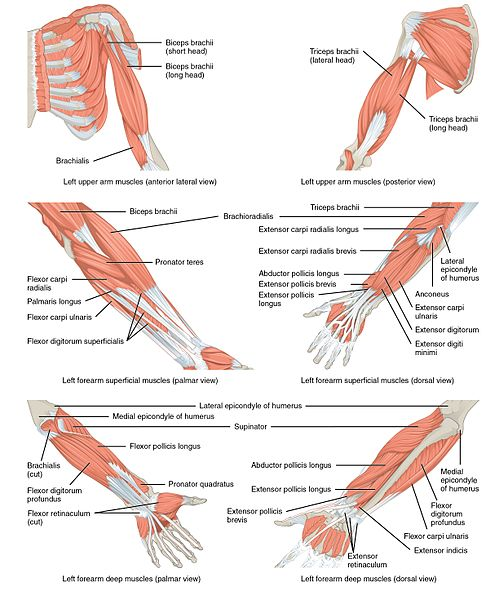
Muscles that Move the Forearm. Public domain Wikipedia CC BY-SA 4.0
Finally the mobile muscle pad is represented by the long supinator, first radial and second radial, does not contain nerves and arteries of relevance.
What happens pathophysiologically?
The initial imbalance of the compartment syndrome is the result of volume and pressure within the closed and unstable myofascial compartment.
This causes arterial perfusion and venous return to decrease significantly proportional to the volume and the pressure increases in the compartment.
Once this happens the blood begins to drift through the capillaries of the muscle tissue, in a compensatory manner, however, it is not very beneficial as it leads to worse tissue oxygenation.
The magnitude of tissue damage is determined by the duration of the ischemia, it is estimated that loss of muscle viability is obtained after 6 to 8 hours of ischemia and loss of nerve viability after 8 hours of complete ischemia.
The decisive factor in the development of compartment syndrome is the alteration of the pressure gradient between the arterial and venous flow. Therefore, the purpose of measuring intercompartmental pressure is to determine the magnitude of ischemia.
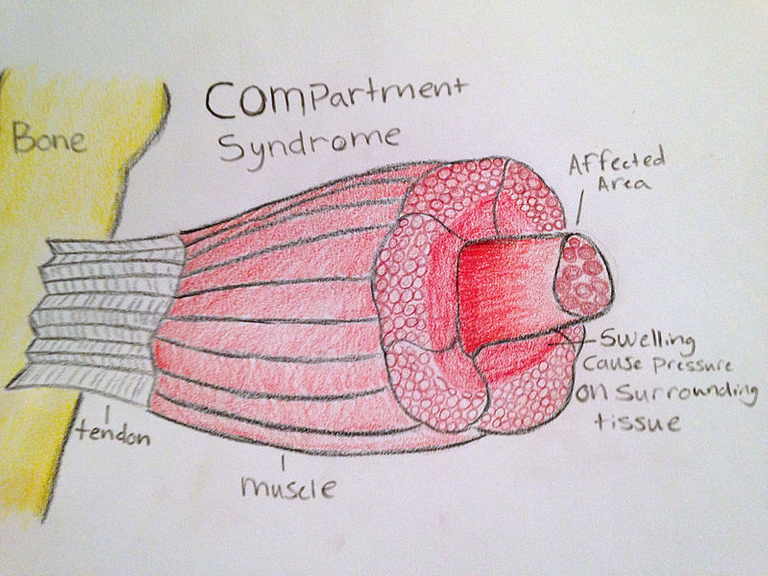
Compartment Syndrome in Muscle. Public domain Wikipedia CC BY-SA 3.0
The normal pressure that should exist in a compartment ranges from 0 to 8 mmHg, with an absolute pressure value of 30 to 35 mmHg. Another alternative to the absolute value calculation, resulting from a measurement between 10 to 30 mmHg above the mean or diastolic blood pressure is an indication of fasciotomy.
However, we must be clear that if the intracompartmental pressure is equal to or greater than 30 mmHg, we must consider that we are in the context of a compartmental syndrome.
Compartment pressure measurement
Who will be performed?
It will be indicated for all patients with increasing pain in a tense and swollen muscle group.
The pain should not be related to an underlying condition such as fracture, contusion, trauma among others. This should increase with the movement of the limb.
The absence of the pulse, the delay in capillary filling and color changes with criteria to perform a compartment pressure measurement.
Will compartmental measurement be contraindicated?
There is no absolute contraindication to perform this technique, in fact, time is of the essence in these cases. Delaying the measurement of intracompartmental pressure and thus its treatment can lead to irreversible damage to the affected limb.
Techniques
Several techniques have been developed to develop compartment pressure measurement. Some use isolated intracompartmental pressure measurements, and another for continuous pressure measurement.
Needle Manometer Technique
We must first develop a simple system that consists of connecting the mouth of a 20 ml syringe to the central connector of a three-step key.
Connect one end of the endovenous extension tube to one of the connectors of the three-way wrench. Place an 18-gauge needle into a container of sterile saline to eliminate the vacuum.
Insert the needle connected to the extension tube into the saline so that the needle hole is well immersed. Open the three-step wrench only for the syringe of the extension tube.
Vacuum saline so that half the length of the intravenous extension tube is filled (check that no bubbles enter the system), turn the key so that the saline connector is closed. Attach another intravenous extension tube to the remaining connector of the three-step or three-way faucet and connect the free end of this tube to a pressure gauge or blood pressure monitor.
Remove the 20ml syringe from the system and suck 15ml of air into the syringe. Reinsert the syringe into the faucet, and remove the intravenous extension tube with the 18-gauge needle from the saline container.
Finally insert the 18-needle into the affected muscle compartment, turn the key so that all 3 connectors are open. Push the plunger of the syringe gradually and gently to increase the pressure inside the system.
The point at which the meniscus is flat and the saline column begins to move is equal to the pressure inside the compartment, let's record and document the pressure of the manometer.
The same needle may be inserted in another location to obtain additional pressure measurements if an asepsis has been followed during the procedure.
Stryker Technique
The Stryker Intracompartmental Monitor System is a suitable, accurate and easy-to-use self-contained device. It consists of a single-patient disposable container, including a needle, diaphragm camera and syringe filled with saline, plus a battery and a digital display.
The steps for assembling the system should be used according to a set of aseptic standards.
First remove the diaphragm chamber from the pressure monitoring equipment container. Place the 18-gauge sterile needle. Uncap the 3 ml syringe filled with salt solution and screw on the other branch of the diaphragm chamber.
Open the clear plastic lid on the monitor unit. Place the needle-diaphragm chamber-syringe assembly on the monitor so that the diaphragm chamber fits into the well.
Carefully push the diaphragm firmly and level on the monitor. Close the lid until you hear a click. Push the plunger of the syringe to pass saline through the diaphragm and needle to ensure there is no air left in the system.
Insert the needle into the desired compartment, slowly inject 0.3 ml of saline into the compartment, which we use to balance with interstitial liquids.
We wait a few seconds until the device gives the result of the pressure and shows it in the digital screen and we proceed to remove the needle.Complications
There should be no complications following the performance of this procedure, provided that asepsis and antisepsis standards have been met.
However, there is a risk that the introduction of a needle into a compartment will trigger local infections or to nerves and vessels.
Obtaining an erroneous intracompartmental pressure measurement leading to unnecessary fasciotomy or even worse that this is not performed and triggers necrosis of the limb.
Multiple pressure measurements must be taken around the affected area as omitting or performing a fasciotomy with a single measurement poses a high risk.
Conclusions
Compartment syndrome is a well known disease, which has been studied very thoroughly in such a way that it is very well documented and described in literature. We must bear in mind that this type of pathological phenomenon presents a clinic that can vary according to the time that elapses.
The determination of the intracompartmental pressure is part of a very important tool for specialists in the medical area to reach a final diagnosis. It should be noted that there are many methods for measuring compartmental pressure, however the most commonly used systems are the conventional manometer and needle system and on the other hand the Stryker system for its simplicity when it comes to perform in an emergency medical area.
Remember that once diagnosed or if the presence of a compartment syndrome is suspected, it is assessed by a specialist traumatologist-orthopedist.
Sources:

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
I hope you enjoyed my content.

Hello,
Your post has been manually curated by a @stem.curate curator.
We are dedicated to supporting great content, like yours on the STEMGeeks tribe.
If you like what we are doing, please show your support as well by following our Steem Auto curation trail.
Please join us on discord.
Thank you very much for supporte @stem.curate
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.
Thank you @steemstem