The next topic I will share is typical in medical emergency rooms, usually patient who comes for the presence of foreign body in your body, being the most common in the skin, is for this reason that attracts note that article, I hope you like it.
Wounds that contain a foreign body represent more than 35% of consultations in emergency areas and sometimes go unnoticed in a first assessment. Cleaning up the affected area is of great help to us.
The presence of an unrecognised foreign body can lead to complications such as infection, loss of function, joint injuries, tenosynovitis, torn tendons and osteomyelitis. Patients who present with a chronic, recurrent, or prolonged skin infection should be evaluated for the presence of a foreign body.
To identify a foreign body, we must have suspicion of its presence, and this will be given according to the interrogation, mechanism of the injury and the physical examination, which will be based on a methodological and careful examination that includes imaging techniques, since the presence of a foreign body is always obvious.
It is important to be familiar with the characteristics of different foreign bodies and the interactions they may cause in a recipient patient. Knowing all this is crucial to determine the urgency or need for extraction (since not every foreign body should be removed). Imaging techniques such as x-rays and ultrasound are very helpful in these cases.
Removing a subcutaneous foreign body can become a frustrating and time-consuming task if not addressed and treated correctly.
Pathogenesis
Only a small percentage of the wounds have a foreign body. As mentioned, the mechanism of the injury, are those that suggest the presence of the same. Wounds caused by puncture or crushing, especially those located on the soles of the feet, deeper than 1 cm, with involvement of subcutaneous cellular tissue, are usually related to the presence of foreign bodies inside them, which are difficult to diagnose and remove.
The risk increases in those injuries where at the moment of being provided by a fragile object that fragments or splinters, during the mechanism of realization of the wound. It is necessary to take into account and explore the presence of pieces of teeth in the lacerations of the face or lip, where there is a fracture of the jaw and involvement of teeth.
Those patients, with a history of intravenous drug use, should explore and rule out the presence of needle portions in skin lesions, secondary to the administration of these substances.
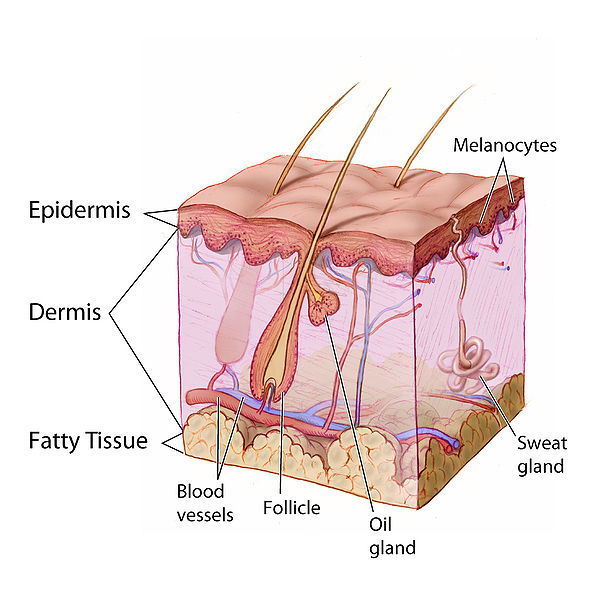
Objects larger than half a centimeter in diameter that penetrate the skin can push any fragment that is thrown in the epidermis layer, towards the interior of the wound, can trigger the formation of a so-called Epidermal Cyst.
The final product of the presence of foreign bodies on the skin is the formation of local foci of infection, where it is typical to observe inflammation of the area, whose severity will depend on the characteristics of the foreign body, either by the material that is constituted, the size, shape and location, which can delay the healing process or can cause greater damage with destruction of adjacent tissues.
The foreign bodies are made up of organic material, such as wood, causing more serious inflammatory reactions, even producing chronic granulomatous reactions, periosteal reactions, osteological, or serious infections such as necrotizing fasciitis.
We must take into account and pay attention to the wounds that do not respond well to the treatment with antibiotic therapy, since it is very probable that a foreign body is thrown inside them and in order to improve it, this object must be removed.
The presence of an object made of lead tends to trigger systemic effects, especially when it comes into contact with pleural or peritoneal fluids, cerebrospinal fluid or intra-articular fluid. While objects with non-porous surfaces, such as glass and plastic, trigger a minimal tissue reaction and when they are not removed or expelled by the body's defences, they end up encapsulating, which will be reduced over time.
Physical evaluation of the patient
Patients who come to the emergency medical unit after an injury require an anamnesis oriented towards the details of the accident, the mechanism of production of the wound and its causal agent. This information will suggest the presence of foreign bodies and will allow us to select the appropriate imaging techniques.
It is essential to determine the presence of pathological antecedents, such as diabetes mellitus, peripheral vascular disease, renal disease, immunosuppressive states, among others, as well as investigate allergic reactions and interactions with certain drugs.
Tetanus immune status should also be confirmed and booster doses of the vaccine should be administered if necessary.
The physical examination begins with a brief inspection, condition, and involvement of the affected skin. The functional part of the affected limb should be carefully examined through flexion and extension movements to evaluate the integrity of the tendons and muscles. Emphasis should be placed on any skin discoloration or pigmentation that may suggest the presence of a foreign body.

Physical exam CC BY-SA 3.0
With respect to palpation, we can only determine the presence of superficial objects, but the presence of acute pain on palpation of a puncture wound suggests the retention of a foreign body, thus meriting the use of local anesthesia for exploration of the wound, where the edges of the wound should be extended with a scalpel and thus broaden and deepen for the exploration of the injury.
One way to explore the wound cavity is to introduce an examiner's finger, protected by a glove, carefully and thoroughly so as not to injure adjacent tissue. If during the exploration we feel the presence of a tear, or the touch of a body of hard consistency, it is very likely that we will not find the presence of a foreign body.

Public domain Flickr
We must avoid taking what we believe to be the presence of a foreign body if we are 100% sure, as this can trigger extensive and even vascular lesions (vessel or artery lesions).
Complementary studies
Imaging techniques are indicated in most cases, when the presence of a foreign body is suspected but not determined during the physical examination, when it is not possible to perform the lesion exploration, or when the patient has the sensation of an unidentifiable foreign body.
Radiography
This technique is very simple and accessible, most of the literature describes the indication of this study, in the presence of any penetrating wound located in extremities.
We suggest performing standard anteroposterior and lateral x-rays, using a low penetration technique for the soft tissues, allowing us to increase the contrast of the foreign body and decrease the contrast of the skin. The visibility of the object will depend on its composition, density, size and orientation in the tissue.
Radio-opaque foreign bodies may go unnoticed when projected onto or impacted by bone. Metal, bone, teeth, pencils, graphite, sand, and aluminum are visible on the x-ray. With regard to most plastics and organic materials this method is not useful.
When there is a high degree of suspicion of the presence of a foreign body that is not visible on the x-ray, more complex studies such as CT and MRI scans should be requested.
The advantages of simple radiography is its low cost, easy access, availability and familiarity for most doctors, among its disadvantages we have the inability to distinguish objects with densities similar to those of tissues, despite its disadvantages remains the method of choice in these cases.
Ultrasound
This method has the ability to locate a foreign body in three dimensions, allowing us to establish its relationship with bone tissue, muscle and tendons, and that in turn avoids the exposure of the patient to radiation, in the case of use of simple x-rays.

Ultrasound. Public domain Flickr
The disadvantage of this method is that it must be carried out by trained personnel and studied in this area in order to establish a reliable diagnosis, and that it does not run the risk of being confused with other structures belonging to the body.
Computerized Tomography
CT images can show us multiple planes and slices, allowing us to quickly, easily and safely identify the presence of a foreign body, even in very important and vital anatomical structures. This technique, in turn, can provide us with a double option, both diagnostic and therapeutic, especially in those cases where the CT is the guiding medium for the extraction of a foreign body, with respect to its disadvantage lies in its high cost, high radiation, availability and availability on the part of the patient.

CAT scan equipment From Wikipedia CC BY-SA 4.0
Magnetic resonance
It is the most precise technique for the identification of wood, glass, plastic and thorns. It is superior to CT for determining infectious processes such as identifying edema, bleeding and infection in the area where the foreign body is located.
Other advantages are its high resolution and high contrast, which allows us to identify foreign bodies in three dimensions and does not expose the patient to radiation. Among its disadvantages it is based on its low availability and high cost.
Its use is contraindicated, in metallic foreign objects, since during its execution iatrogeny can originate, especially if it is located in the eyeball.
Indications
Every effort should be made to identify a foreign body, even if it cannot be removed. A decision should be made whether, once a foreign body has been identified, it should be removed immediately, on an elective basis, or not at all.
The factors that influence the removal of a foreign body are based on the size, composition, its proximity to vital structures and associated injuries.
Contaminated objects such as teeth, soil, toxins, which trigger bleeding or ischemia should be removed immediately. Objects that alter the motor or sensory function of the affected limb should also be removed.
Most foreign bodies located in the hands or feet require removal because they tend to injure nerve endings and tendons over time.
Contraindications
All those injuries should be referred to a specialized service, either General Surgery, Plastic Surgery or Traumatology, which are located near the tendons, nerves and blood vessels.
In relation to large, deep and embedded objects that are created by covering the wound, they should not be removed, only by a specialist and in an operating room.
Finally, foreign bodies associated with fractures or located in joints require surgical cleaning because of their high risk of complications such as osteomyelitis.
Preparing the patient
Removing a foreign body can be a frustrating and time-consuming process, even though I know that it is done under ideal conditions. Therefore, consider a time limit of 10 to 30 minutes to remove the object, and when this limit is exceeded, it is advisable to refer to a specialist.
Measures of asepsis and antisepsis of the affected area should be carried out, with extreme care, avoiding deepening and adhering to deeper planes in the foreign body.
Place a pressure cuff near the lesion, elevate the limb and proceed to inflate the cuff, which will serve as a vasoconstriction and safety measure to control and prevent bleeding.
It is advisable to place local anesthesia, which will facilitate the removal of the object.
Techniques
Extraction of surface wood or organic chips
In most cases, it is difficult to visualize small objects. A reasonable method is to carefully smear soap solution and remove foreign bodies and splinters on the surface of the skin with tweezers.
When the object takes on a deeper layer and is located parallel to the skin, an incision should be made and the foreign body removed with a haemostatic forceps.
Puncture wounds
This type of wound is very common in feet, and is associated with the introduction of fabric, parts of footwear or any other fragment inside the wound, which increases the risk of infection from this type of injury. In these cases, irrigation and debridement of the wound are beneficial.
In those cases where irrigation and debridement is not enough, the injury should be enlarged with a scalpel blade, making an ellipsoidal incision in the skin surrounding the foreign body, removing the skin portion and separating it from the underlying dermal tissue, visualizing the foreign body and extracting it.
Another alternative is to make a linear puncture incision 1 mm away from the foreign body, carefully widen the incision and visualize and remove the object.
Finally, it is feasible to make a linear puncture incision over the foreign body. Separate the edges of the incision and put pressure on them so that the foreign body is pushed out and taken up with a forceps.
Staining technique to locate a needle
It is very helpful in methylene blue in these cases, we must be sure of the presence of the needle in the body either by a simple x-ray or any other technique. Clean and prepare the skin by injecting approximately 0.3 ml of methylene blue through the entry hole of the foreign body, which will highlight the path the foreign body took and finally its location.
Finally, an A-U V or Y-shaped incision is recommended over the entry point and lift a piece of tissue. Once the location of the object is identified by the methylene blue, it is removed from the lesion.
Sometimes this technique is complicated because the ink infiltrates through the tissue.
After care
Subsequent x-rays are recommended to confirm that the foreign body was completely and satisfactorily removed.
Perform outpatient irrigation and subsequent cleaning of the wound once the foreign body is removed, preventing infection.
In cases of deep wounds with abundant material and foreign bodies, it is not recommended to close the wound through sutures, but to continue with irrigation.
The use of antibiotics is recommended both for the manipulation of the area, extraction of tissue, as well as for the overinfection product of the foreign body.
Tetanus prophylaxis
Always recommended, especially those wounds contaminated with saliva, feces, soil, metal, missile products, and burns.
Sources:

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
If you have any questions about any topic of medicine or present any disease you can comment the publication or write me in discord and I will attend you.
Dr. Ana EstradaI hope you enjoyed my content.


)

@tipu curate
Upvoted 👌 (Mana: 20/30 - need recharge?)
Thank you @girolamomarotta
Great job, as always ✌️
This post has been voted on by the SteemSTEM curation team
and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.
Thank you very much for the great support always @steemstem
Your level lowered and you are now a Red Fish!@anaestrada12, sorry to see you have less Steem Power.
Thank you @steemitboard
Those pictures are not so great to look at after dinner... I am pretty sure to have already said that to you in the past ;)
Anyways, nice article. I remember having held lab classes for master students in nuclear medicine about tomography (we have a very simplified device they could use as an illustration to the key physical principles behind it).
Oh, sorry I forgot to leave a note about the pictures at the beginning of the publication. I hope it didn't spoil your appetite :)
Really, I placed the images of the equipments just so that it would have a relation with what I was writing.
I don't know anything about physics, I've always been bad, very bad. :)
That is fine, I can take a lot ;)