Evolution of Brachytherapy.
After the First World War, different Brachytherapy schools were created: the Hemmet Radio in Stockholm, the Memorial Hospital in New York, Regaud Lacassagne and the Radio Institute in Paris. Progressively the foundations of Brachytherapy were established. The methods of Stockholm and Paris for procedures in intracavitary treatments were developed in 1914 and 1919. In the 1930s they were published by Patterson and Parker and later by Meredith the rules of the Manchester System for interstitial treatments with Radio [1].
The Cobalt needles were used for a short time after the Second World War, falling into disuse like Tantalum and Radioactive Gold, mainly due to its long half-life which made it difficult to recover it over time [1 ] Iridium was used for the first time by Henschke in 1958 and since then it is still the most used artificial radioactive source in Brachytherapy [1].
Definition.
Etymologically the word Brachyrapia comes from the Greek "brachys" which means "close". Also called short-distance therapy, which is a radiotherapy treatment method in which sealed radioactive sources are used to administer radiation doses at close range of a tumor, either interstitially, intracavitatively or intraluminally and superficially. With this Radiotherapy mode, a high dose of radiation is delivered locally to the tumor and due to its high dose gradient, the damage to the surrounding normal tissue is very low since the radiation rapidly decreases at a short distance from the tumor.
Implementation Techniques.
Brachytherapy is applied through the introduction of artificial isotopes in deferred charging devices with remote automatic controls, thereby reducing the exposure of personnel and can safely perform exposures of low, medium and high activity radiation sources of a controlled way. Although external beam radiation treatments are often used as an alternative to interstitial implants, Brachytherapy remains an important modality of therapy, either as monotherapy or as an adjunct to external beams. [2], [3] and [1].
Figure 1 shows examples of the most common Brachytherapy implants today for cancers with higher prevalence and morbidity and mortality: prostate, cervix, endometrium, bladder, breast and brain, in addition to some rare types such as bile ducts, neck, tongue among others.
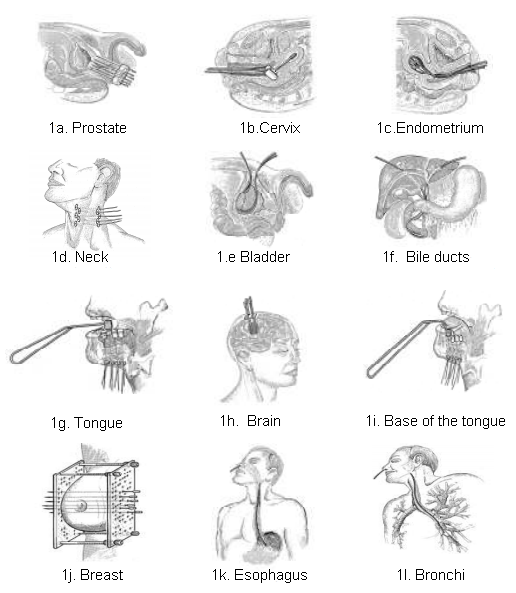
Figure 1. Different types of implants with Brachytherapy [4].
Next, the three types of Brachytherapy are explained according to the type of implant:
Surface Therapy through molds.
Plastic molds adjusted to the surface to be irradiated can be prepared and the sources are placed side by side on the outer surface of the mold. The distance between the plane of the sources to the surface of the skin is chosen fulfilling criteria such as size and depth of the tumor so that the dose delivered to the tumor is ideal for treatment without damaging adjacent healthy tissues, these distances are usually from 0.5 to 1.0 cm.
Interstitial therapy.
Here, the applicator used is needle-shaped, which is inserted directly into the tissue. There are basically two types of interstitial implants: temporary and permanent ones. In a temporary implant, the sources are removed after the desired dose has been administered (for example, radio needles, wires or iridium seeds). In a permanent implant, the sources remain permanently in the implanted tissues (for example, seeds of 198Au and 125I).
Intracavitary Therapy.
Intracavitary therapy is used primarily for cancers of the cervix, body of the uterus and vagina. Some varieties of applicators have been designed to have the radioactive sources in a fixed configuration, guaranteeing reproducibility and constancy in the treatment. A cervical applicator, basically, consists of a central tube, called a tandem and two lateral ovoids, among the most common we have: the Manchester applicator, Fletcher and Stockholm which have a provision for sources of cesium and iridium can work with low, medium and high dose rate in Figure 2.

Figure 2. Applicators used in intracavitary brachytherapy: a. Manchester, b. Fletcher and c. Stockholm [5].
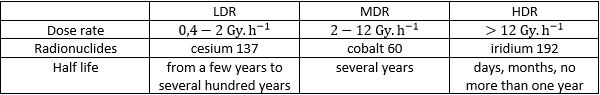
Brachytherapy according to the dose rate.
Since the beginning, Brachytherapy has worked with different types of radioactive sources (Radio, cobalt-60, iridium-192, among others) which, depending on the rhythm of the dose arrangement, that is, the dose rate ( Gy / h) supplied by the source during treatment can be classified into low, medium and high dose rate [3]. The following table establishes a comparison between the different types.
Reference.
[1] Khan, & Faiz, M. (2010). The Physics of Radiation Therapy. Minneapolis Minnesota.
[2] Bethesda. (1997). Dose and volume specification for reporting interstitial therapyin gynecology. ICRU Report 38.
[3] ICRU. (1985). Dose volume specification for reporting intracavitary therapy in gynecology. Report 38. Washigton.
[4] An Eckert & Siegler Company. (2010). Afterloading Multi & Gyne Source. Bebig: Zubehör/accessories.
[5] Gerbaulet, J., Pötter, R., Mazeron, J., Meertens, H., & Van Limbergen, E. (2008). The GEC ESTRO Handbook of Brachytherapy. ESTRO ISBN.
[6] IAEA. (2003). Radiation Oncology Physics: A Handbook for Teachers and Students. Vienna: STI/PUB/1196. IAEA.
Very interesting post. Congrats! And thank you for sharing this info.