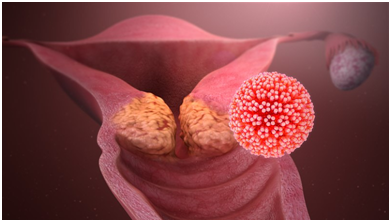
Human Papillomavirus (HPV) is the cause of one of the most common sexually transmitted diseases (STDs), and is also the main risk factor for the development of uterine cancer in the women; It is therefore an etiological agent of great relevance in the world, in relation to the prevalence of important diseases.
However, although there are more than 100 different genotypes of this virus, only a few constitute a real risk, being able to cause clinical disease.
To understand a little better about the development of these pathologies, it is important to know a little more about the virus itself; Since, as the title of the article emphasizes, this constitutes a silent threat at present, due to its high prevalence, and in contrast to it, the little information that the population in general handles on the subject.
What kind of Virus are we talking about?
These are small DNA viruses, belonging to the Papovaviridae family, called Papillomavirus (PV), which are capable of infecting a wide variety of vertebrates, including humans.
They are of an approximate size of 5nm in diameter, and lack a membrane.
Although they are widely distributed, they show a high degree of cell tropism: what does this mean? Well, they only infect specific cell types, in this case, dry epithelia (such as the skin), and mucous membranes (either oral and / or genitals), leading to the development of benign lesions (called warts or papillomas), and under certain conditions and in association with certain risk factors, they can cause carcinomas.
Since 1976 when Harald Hausen, for the first time described this family of viruses, numerous clinical, molecular and epidemiological studies have been carried out, which until now, continue to show the HPV as the main etiological agent of cervical cancer.
More than one hundred types of HPV have been identified, and more than twenty types are associated with infection in humans, these have been subdivided into 3 groups, depending on the level of risk they represent.
Source: Wikipedia. Papillomavirus (HPV)

There are about 200 genotypes of the human papillomavirus, 30 of which types are responsible for ano-genital infections.
Depending on the potential for malignancy, each subtype of HPV is classified into any of the following 3 groups:
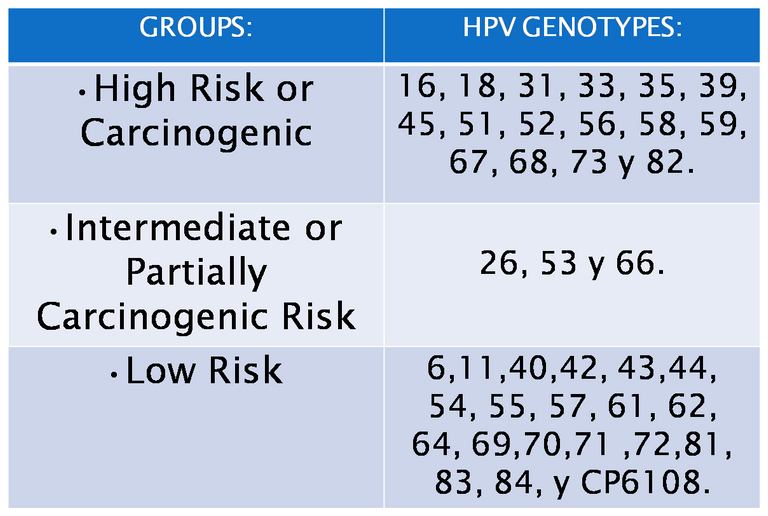
Types 16 and 18 are the most frequently related to cervical, vulvar, penile and anal cancer.
While types 6 and 11 are more associated with the development of benign lesions such as warts and illuminated condylomas.
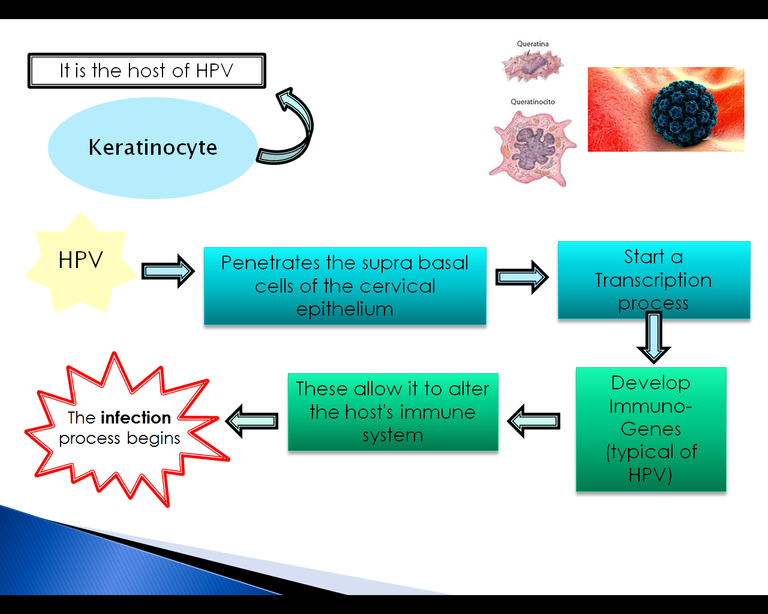
In the pathogenic process that involves virus infection and the consequent presence of diseases, many factors are included; highlighting important factors in host resistance, mediated by T lymphocytes, the process of cellular necrosis (which are observed at the site of regression of the lesions), as well as the participation of antigen presenting cells, and performance of pro-inflammatory cytokines.
However, factors specific to the virus come into action, to deal with the body's defense mechanisms, and certain virulent factors allow it to bend the efforts of the immune system to defend ourselves, and thus manage to develop the infection.
The pathophysiological process of virus performance is summarized in the following image:
How is the infection transmitted?
The route of transmission of epithelial HPVs is from person-person through direct contact with infected skin areas.
Genital HPVs are basically transmitted by sexually (vaginal, anal or oral); and other forms of contagion have also been suggested such as the use of instruments and through fomites, however, these do not seem to be significant.
More recently, placental transmission (although very infrequently) has been demonstrated in children born by natural delivery of patients carrying the virus, producing laryngeal papillomas.
However, it is true that there are certain predisposing factors that facilitate the development of infection and disease by these viruses. These risk factors are summarized in the following image:
We see how risk factors are mainly related to promiscuity and the early or early onset of sexual activity; However, it is important to highlight that anyone who has had sexual contact with another individual is at risk of becoming infected with this virus (regardless of their age or number of previous partners); Its high prevalence is related to the fact that both men and women can get the virus and transmit it, without knowing it.
Low social conditions are also considered as a risk factor, because it has been shown that it is a disease highly linked to underdeveloped countries, being especially prevalent among the poorest population.
Likewise, sex education plays a fundamental role in relation to the development of this type of pathologies; since STDs are becoming more frequent among adolescents due to the early onset of sexual activity without any orientation. It is our duty as adults, to echo the information necessary for sexual activity in young people to be safe, and thus reduce the risk of these diseases.
As already mentioned above, it is an infection that can affect both men and women, and in a large percentage of cases it is asymptomatic; However, these people become part of the "carrier" population of the virus, and can transmit it to other people, even without knowing it.
In infected people, different courses could be presented: the virus could be eliminated by the person's immune system, without presenting any damage and in a rapid period, so the person would not transmit the infection to others for a long time; The immune system manages to control but DO NOT eliminate the virus from the organism, so the person probably does NOT develop clinical disease, but would be an asymptomatic carrier of the virus, however this will not prevent him from transmitting it through the contact, to healthy people; In the rest of the cases, the body's defenses are not enough to prevent the spread and damage caused by the virus, so there is the development of typical lesions, whose location and characteristics will depend on the viral genotype involved in each case.
This is explained by the fact that it has been shown that certain types of viruses are related to specific lesions, as well as in Venezuela, serotypes 16, 18, 33, and 45 produce 80% of cases of cervical cancer, and between 40-70% of moderate and high grade cervical lesions; while viruses 6 and 11 are the most related to the appearance of warts (which are in turn, the most common lesions in males).
When to suspect that you have an HPV infection?
It is important to know how to recognize the symptoms and signs that can alert us to a possible HPV infection; as in all STDs, the sexual antecedent is essential, and this can also be accompanied by:
If the person does NOT go to the doctor and does NOT receive any treatment, the course of the lesions can be varied: they can disappear, remain unchanged, or on the contrary grow and / or multiply. An important fact to know and take into account, is that genital warts do NOT turn into cancer.
What is the risk of developing Uterine Cancer after HPV infection?
The evolution of a moderate-high risk cervical lesion to cervical cancer is based on the progressive development of the lesions, which consists of several stages.
First there are histological changes at the level of the cells that make up the cervix, these abnormalities are known as: Cervical Intraepithelial Neoplasia (CIN), and depending on the degree of involvement this can be type I or II; the considered ‘CIN III’ is already an in situ cancer, which can eventually progress to an invasive cancer.
Epidemiological studies carried out based on this pathology show that approximately 85% of severe histological alterations (CIN II onwards) present the DNA of the virus, while 100% of invasive cancers present the virus.
It is for this reason that the timely diagnosis of these histological alterations is essential to prevent their progress to in situ and / or invasive cancers. For this purpose there is the Pap test (cytology), which allows us to evaluate the cellular changes produced by HPV, and can detect them early, in order to treat the cervix before the cells become cancerous.

As just mentioned, the Cytology or Pap Test, allows us to identify epithelial changes produced at the level of the patient's cervix, and it is also a test that every woman should perform periodically (being indicated every three years in all sexually active women, and every year if the previous test showed any abnormal results).
However, this test is not specific for the virus as such, since for this there are more specific tests and that are indicated to make an isolation and identification of the virus.
During a first phase of latent infection, in which the patient does not present any type of clinical manifestation, but a viral replication process is being carried out within his organism; The virus can be identified through the Polymerase Chain Reaction (PCR) test, which is a molecular biology technique.
Subsequently, there is a subclinical infection phase, since the virus at this time has caused small microscopic changes in the cervix cells (coilocitic changes or dysplasias) which can be diagnosed through: routine cytologies, biopsies of the tissue; or macroscopic changes can also be observed through the gynecological examination, with the use of a solution with iodine or acetic acid (where color changes are highly suggestive of the presence of a pre-malignant lesion).
Finally, those patients with clinical infection, such as warts, their diagnosis is carried out through physical examination during medical consultation. And those patients with the presence of malignant tumors, the previous tests are useful to carry out a diagnosis: being the BIOPSY of affected tissue the method of lesson and definitive diagnosis of cancer.
Can HPV infection be prevented?
The safest way to prevent an HPV infection is through responsible sexual activity, limiting the number of partners and using condoms in each case.
Currently there are three vaccines for primary prevention against HPV, which is indicated mainly in girls between 11-12 years of age (since it is sought to comply with the doses before the onset of sexual activity); and the main objective of this vaccine is to reduce the incidence of this infection to prevent the development of uterine cancer.
These vaccines are:
Bivalent Vaccine: protects against serotypes 16 and 18.
Tetravalent Vaccine: protects against serotypes 16, 18 and also 6 and 11 (the viruses responsible for the appearance of warts, so it is the vaccine placed in ** men **).
Nanovalent Vaccine: protects against serotypes 6, 11, 16, 18, 31, 33, 45, 52 and 58.

Although there is currently no definitive or specific treatment for HPV, it is sought to give better quality of life to patients infected by this virus, always taking into account the extent and morphological characteristics of the lesion, in order to give them timely treatment
It's very important, as in any pathology, to make an individualization of each patient, since the treatment of each case will depend on the form of clinical presentation, as well as the location and other characteristics of the lesion; the above added to the patient's own factors, such as sex, age, comorbidities and adherence to treatment.
There is a wide variety of therapeutic possibilities that include:
Chemical therapies: they act through cytotoxicity.
Topical medications: Tridoracetic acid and the anti-metabolite 5-fluoracil.
Antifungal agents: Podophyllin-podophyllotoxin.
Methods that allow the destruction of damaged tissue, which include: Cryotherapy, Diathermic electrocoagulation, CO2 Laser Vaporization, Thermocoagulation.
Use of certain antivirals and immunoregulators.
CONCLUSIONS:
The Human Papillomavirus is the etiologic agent of one of the most frequent sexually transmitted diseases in the world, whose high prevalence is strongly linked to irresponsible or promiscuous sexual activity, and which can affect both men and women; It is also a very high risk factor for the subsequent development of cervical cancer.
It is for these reasons that early sex education is a fundamental key in the prevention of these pathologies; while the vaccines that currently exist, represent another important prevention measure.
It should be sought as far as possible, to promote responsible and safe sexual activity, as well as information related to the subject, which allows the population to be updated based on the severity of this pathology.
Bibliographic References:
[1] Human Papillomavirus: Literature Review. Vasquez-Bonilla
[2] Human papillomavirus: Virological and immune aspects A. Alba Menéndez.
[3] Genital Human Papillomavirus: THE REALITY. U.S. Department of Health and Human Services
[4] Human papillomavirus (HPV). FDA Office of Women's Health.
[5] Rodríguez González D, Pérez Piñero J, Sarduy Nápoles M. Human papillomavirus infection in middle-aged women and associated factors. Rev Cuba Obstet Ginecol. June 2014.
[6] Concha P X, Urrutia S T, Riquelme H G. Beliefs and human papillomavirus. Rev Chil Obstet Ginecol. 2012.
[7] Muñoz N, Bosch FX, from Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003.
Hello everyone! Thank you very much for reading me, especially to the scientific community on Steemit.
This time I wanted to make this article based on the high prevalence of this disease in Latin American countries, with the intention of always providing good content and relevant information that allows us to continue nurturing our knowledge.
I previously published this article in Spanish, but it seemed appropriate to publish it now in English to be able to inform more people about this pathology.
I hope you liked it, you are welcome to leave your doubts / questions / suggestions in the comments, thanks in advance.

I wish everyone would read this article. I like so much about it. First of all, it is highly specific and yet very accessible to the lay reader (me). The chart that shows the different strains of virus and relative risk for development of cancer--that could be very helpful to people who have been diagnosed. Helpful in that at least they can assess their level of risk.
Also, I'm appalled that one path of transmission is 'instrument'. I presume this means medical instrument, as has been the case with certain GI procedures. I don't think this is an acceptable risk. Whether it is a matter of economics (reusing instruments) or poor sterilization...IMHO, this risk simply should not exist.
I believe this is the first article I've by you @iradyjr...I'm a fan now:)
hello, really a beautiful article! it deals with themes that are very dear to me and with a really very comprehensive style but with a simple language, I really liked it, I give you the highest grade and I invite you to join the community of stem.curate, you will find in the next comment the information if you want to come and visit us!
a big greeting,
riccc96
Hello,
Your post has been manually curated by a @stem.curate curator.
We are dedicated to supporting great content, like yours on the STEMGeeks tribe.
Please join us on discord.
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Please consider using the steemstem.io app and/or including @steemstem in the list of beneficiaries of this post. This could yield a stronger support from SteemSTEM.