In primary intestinal pseudoobstruction, the intestine is unable to contract and push food, feces and air through the gastrointestinal tract. The disorder almost always affects the small intestine, but it can also occur in the large intestine.
The condition can appear suddenly (acute) or over time (chronic) and is more common in children and the elderly. The cause of the problem is unknown; therefore, it is also called idiopathic intestinal pseudoobstruction (idiopathic means that it occurs without a known reason).
Risk factors include:Cerebral palsy or other nervous system disorders (neurological). Heart, lung or chronic kidney disease. Stay in bed for prolonged periods (prostrate). Take narcotic pain medications or other medications that reduce bowel movements (often called anticholinergics).

Symptoms: abdominal pain, bloating, constipation, nausea and vomiting, swollen abdomen (abdominal distension), weight loss.
Tests and exams. During a physical examination, the doctor will usually observe abdominal distension.

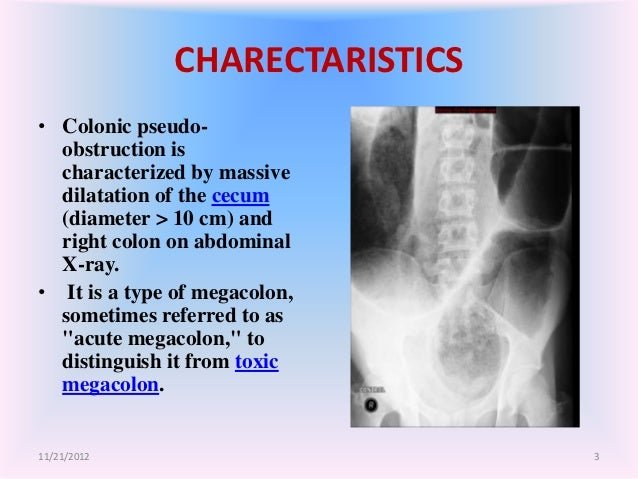
The exams include:Abdominal radiography, anal manometry, esophagography, esophagogastroduodenal transit or opaque enema, blood tests for vitamin or nutritional deficiencies, colonoscopy, computed tomography (CT), antroduodenal manometry, gammagraphy of gastric emptying with radionuclides and intestinal scintigraphy with radionuclides.
Treatment. A colonoscopy may be used to remove air from the large intestine. Fluids can be taken through a vein (intravenous) to replace fluids lost due to vomiting or diarrhea. Nasogastric suction involves placing a nasogastric tube through the nose into the stomach to extract air (decompress) from the intestine. Neostigmine can be used to treat an intestinal pseudo-obstruction that is only in the large intestine (Ogilvie syndrome).
Special diets usually do not work; however, supplements of vitamin B12 and other vitamins should be used for patients with vitamin deficiency. Stopping medications that may have caused the problem (such as a narcotic drug) may help. In severe cases, surgery may be required.
Expectations (prognosis) Most cases of acute pseudo-obstruction improve in a few days with treatment. In chronic forms of the disease, the symptoms may return and worsen for many years.
Possible complications. Diarrhea, rupture (perforation) of the intestine, vitamin deficiency, weight loss.
When to contact a medical professional? Call your health care provider if you have stomach pain that does not go away or other symptoms of this disorder.


https://es.wikipedia.org/wiki/Pseudoobstrucci%C3%B3n_intestinal
https://es.wikipedia.org/wiki/Pseudoobstrucci%C3%B3n_intestinal