Hey Steemit!
This time I would like to share about one of the most commonest and yet merciless disease in the world, Diabetes Mellitus. Everyone knows about Diabetes. It's so common nowadays. Living in Malaysia where food is abundant and tasty, this condition arises from unhealthy diet and sedentary lifestyle. I have yet to find someone that has absolute no family relatives affected with Diabetes.
Type 2 Diabetes Mellitus is a prevalent non-communicable disease which has an increasing trend all over the world. T2DM is very common. The global prevalence of diabetes among adults over 18 years of age has almost doubled from 4.7% in 1980 to 8.5% in 2014, based on the statistics researched by the World Health Organization. That’s almost 1 out of 10 people that you see daily. The statistics result is more worrying among Asian as the ratio is much higher compared to those residing in the West. T2DM is a chronic disease, which is primarily caused by resistance to insulin action as well as relative insulin deficiency. Complications of diabetes mellitus can be divided into acute and chronic complications
Acute:
- Hypoglycaemia
- Hyperglycaemic States (Diabetic Ketoacidosis, Hyperglycaemic Hyperosmolar State)
- Microbial Infections
Chronic:
- Macrovascular (cardiovascular, cerebrovascular, peripheral vascular diseases)
- Microvascular (retinopathy, nephropathy and neuropathy)
Screening and monitoring of the disease is much required nowadays as the amount of ‘victims’ are mushrooming in an alarming rate. Hyperglycemia, or above-normal glucose level has detrimental effects on health. Furthermore, blood glucose level increases with age, indicating that glucose control is essential especially in older population. One of the most popular method to screen and to monitor sugar control is via HbA1c.
HbA1c

According to the report written by WHO, the potential utility of HbA1c in diabetic care is first mentioned in the 1985 WHO report. Glycated hemoglobin or HbA1c, was initially identified as an “unusual” hemoglobin among diabetic patients over 40 years ago. Subsequently, various small studies were conducted in order to find the correlation between HbA1c and sugar control as the world was in a dire need for an ideal method. There was study before which involved 643 participants representing a range of HbA1c levels and this study established the ultimate correlation between those two parameters. In the 1980s, HbA1c was finally introduced into clinical use and the world certainly appreciates it as complications of prolonged hyperglycemia can be brutal and life-debilitating.
What is hemoglobin-A-1-C?
Hemoglobin is the iron-containing oxygen transport metalloprotein in the red blood cells. I bet many of you know about its primary function, which is to carry and distribute oxygen throughout the whole body. Healthy individuals contain approximately 12-16 grams per dL of hemoglobin in their blood. Apart from oxygen, hemoglobin even carries carbon dioxide (as carbahemoglobin) and nitric oxide.
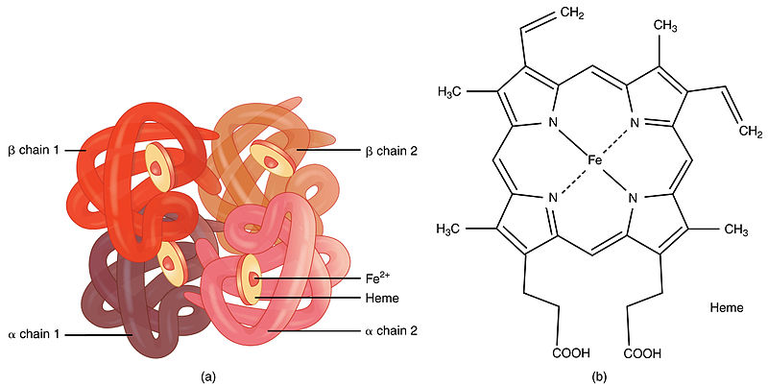
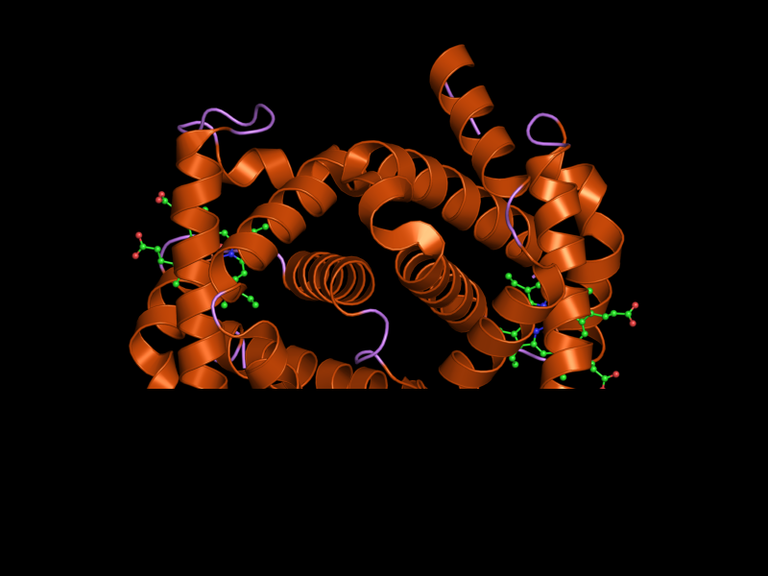
Hemoglobin has a tetramer (four) structure and it is made of many multi-subunit globular proteins. Each subunit contains a protein-chain bound to a non-protein heme group. A heme group is consist of iron (Fe) iron held in a heterocyclic ring, porphyrin. The iron part of the hemoglobin is responsible for the oxygen binding physiology. Thus in patients with low hemoglobin level, doctors often prescribe iron supplementation to aid the hemoglobin production. What about carbon dioxide? Yes, it is carried by the hemoglobin but it does not compete with the oxygen binding site as it binds to the protein chains instead of the heme.
There are a few types of Hemoglobin in humans such as Hemoglobin A (the most common one) and it is made of two alpha and two beta subunits, each made of 141 and 146 amino acids residue, respectively. Other types of hemoglobin include the HbF, which is the primary type of hemoglobin in infants. They are made of 2 alpha and two gamma chains, which is slightly different in comparison with the adult’s one. The gamma chains are gradually replaced with the adult variant as the infant grows. In certain diseased related to the hemoglobins such as Beta Thalassemia, their body can’t produce proper Beta chains. This will result in anemia (low hemoglobin level in the blood) as normal HbA can’t be formed. Individuals with Thalassemia have higher HbF level to compensate the inadequate production of HbA. This clinical situation is significant in HbA1c as individuals with hemoglobinopathies such as Thalassemia might find their HbA1c measurements to be inaccurate.
Hemoglobin A binds to glucose at the terminal valine (a type of amino acid) of each B-chains, which explains the name HbA. In the late 1950s, about 6% of total HbA is termed HbA1, which in then subdivides into HbA1a1, HbA1a2, HbA1b and HbA1c. These fractions are defined by their electrophoretic and chromatographic properties. HbA1c is the most abundant of these fractions and comprises approximately 5% of the total HbA population. Based on the study which I have explained earlier, results showed that people with poor sugar control have higher value of HbA1c.How does glucose and HbA molecules are related?
Glucose molecule attaches itself to the hemoglobin, and this process in known as glycosylation. The amount of Hemoglobin that will form HbA1c is dependent on three factors: concentration of glucose, length of time, and chemical reactions.
1) Concentration of glucose
Unlike many other cells which require insulin for reuptake of glucose, red blood cells are insulin independent. Which means, it does not require any glucose transporters for it to be able to take on glucose. It is very simple here because the higher the blood glucose level, the more saturated the hemoglobin will be, and thus more glycosylation process will take place.
2)The length of time of exposure
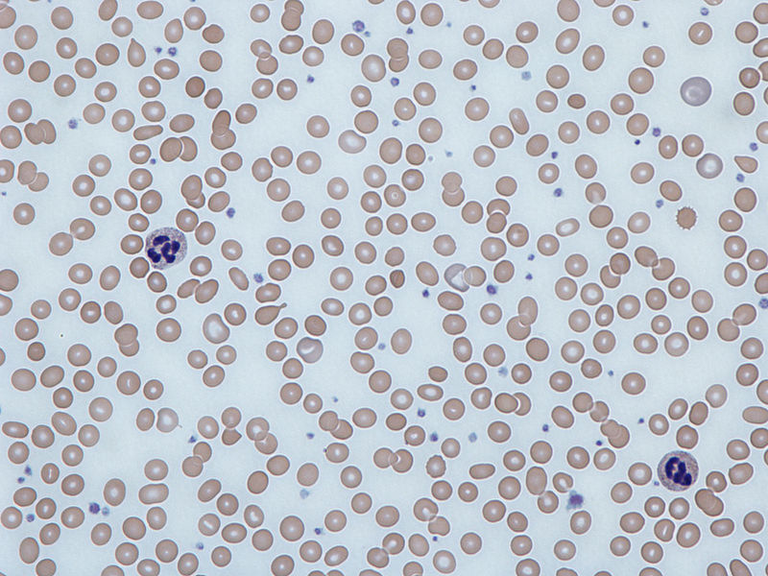
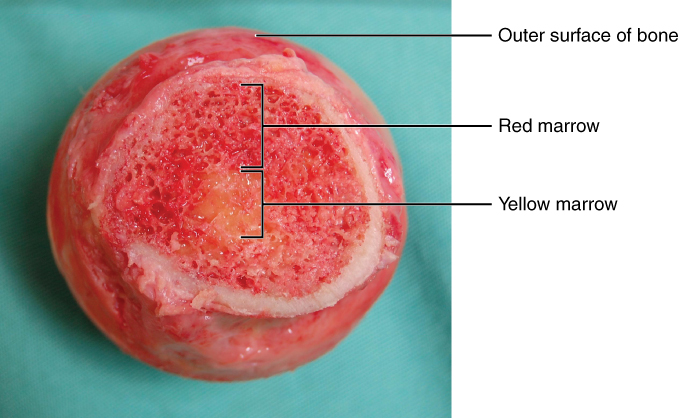
The longer the blood glucose level is high, the more glycosylation will occur. Furthermore, this factor is influenced by the age of red blood cells. The average lifespan of red blood cell is about 120 days. The creation of RBC required approximately 7 days and the process is known as erythropoiesis. The red bone marrow of large bones are responsible in manufacturing new red blood cells to replace the old ones. The production is accelerated with the hormone erythropoietin which is secreted by the kidneys. Hence, individuals with chronic kidney failure demands iron supplementation or exogenous erythropoietin to enhance erythropoiesis. The new red blood cells produced are known as reticulocytes which makes up about 1% of the total circulating red blood cells.
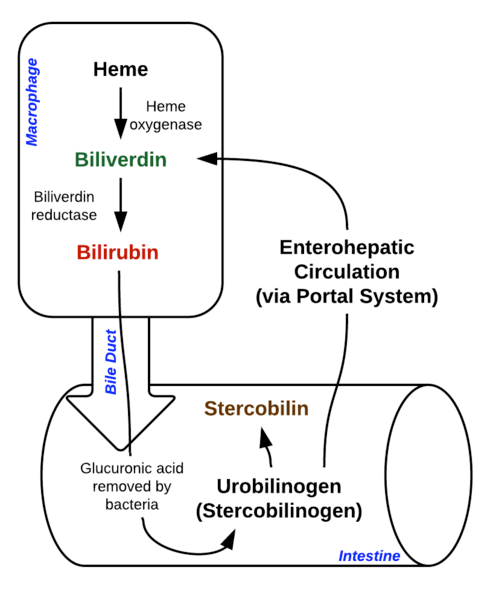
Eryptosis is term used to describe red blood cell death. After it gets old, the structure of RBC undergoes changes to make it more susceptible for macrophages to destroy it. Much of the resulting breakdown products are recirculated in the blood vessels. The heme part is broken down to iron and biliverdin. The biliverdin is reduced to bilirubin. Take note that bilirubin is yellow in colour, and individuals with excess bilirubin which appears yellowish is called as jaundice. Excess red blood cell destruction or immature liver can cause whooping level of bilirubin. The free iron is carried by transferrin. Based on these long explanation, one can guess that diseases that causes the RBC to die faster (or shorter lifespan) makes HbA1c level inaccurate in monitoring their sugar control such as in Hemolytic Anemias.
It has been suggested that half of an HbA1c value is attributable to the previous month, a further quarter to the month before that, and the remaining quarter to the two months before that. Keep in mind that HbA1c usually reflects the glucose control for the past 90 days. RBC life span is 120 days, so where does the 30 days go? Bear in mind that very young and old red blood cells are incapable of binding to glucose as efficient as the healthy red blood cells. Thus, HbA1c level is only capable of determining the sugar control for the past 3 months.
3) Chemical reaction
The actual chemical reaction that binds glucose to the protein is complex. In the short term, an intermediate may form which then dissociate into protein and glucose again. However after some time, the intermediate product undergoes rearrangement and becomes a stable entity. The conclusion is that, during the initial phase, the binding of glucose and protein is reversible at first but overall it is irreversible.
How does HbA1c level measured?
There are several ways in which HbA1c level can be measured, namely the Cation Exchange Chromatography, Affinity Chromatography, Immunoassay and Capillary Electrophoresis. These methods make use the difference between charges of glycated and non glycated hemoglobin. Majority of laboratories are using the cation-exchange high performance liquid chromatography to estimate HbA1c level. Glycated and non-glycated hemoglobin have a subtle difference in their isoelectric points and can be separated on this basis. Cation-exchange chromatography is a chromatography (lab technique to separate mixture) that separates ions and polar molecules based on their affinity.
What could cause HbA1c level inaccurate in determining glucose control?
Every test is imperfect. Scientists are striving to find the best test available that is not expensive, high sensitivity and specificity, fewer contraindications and at the same time non-invasive to the tested individuals. These qualities make the investigation the ideal one. Despite the great introduction of HbA1c, it comes with flaws too.
- Individuals with iron, folate or B12 deficiency has falsely high HbA1c level. This fact arises from the disproportionately high old red blood cells as they are needed in the body still. Iron, folate and B12 are required to synthesize normal hemoglobin. Hence, individuals with either of these conditions tend to have more of their old hemoglobin circulating which results in falsely high number of HbA1c.
On the other hand, individuals with high red cell turnover rate as I’ve mentioned earlier (RBC with shorter lifespan) have falsely low HbA1c due to the enormous amount of young red blood cells. Examples of these individuals are those who is taking iron, B12 and folate supplements and also individuals that is treated with erythropoietin.
The HbA1c values may be falsely high in individuals with abnormal hemoglobins such as hemoglobin F (HbF) or low with hemoglobin S (HbS). High HbF level is associated with Thalassemia and high HbS level in Sickle Cell Anemia.
HbA1c values may be falsely elevated or decreased in those with chronic kidney disease as it interferes with the erythropoietin production.
Individuals taking medication that may cause rapid glucose rise such as Steroids or Atypical Anti-psychotics.
Individuals with pancreatic damage, rheumatoid arthritis, or post splenectomy as they can affect the results of HbA1c.
In addition, HbA1c do not capture hypoglycemic events which makes self-monitoring of blood glucose much superior in this case. Hypoglycemic states can be either due to poor meal timing or too much insulin injections.
HbA1c is not suitable to be used for the diagnosis of diabetes in children, gestational diabetes and type 1 diabetes.
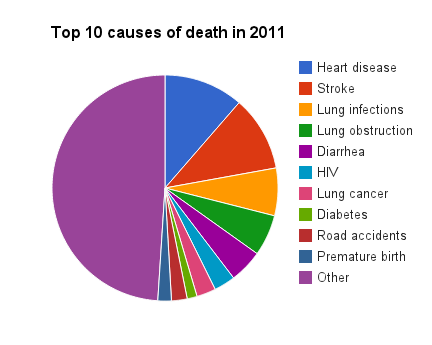
Regardless what, HbA1c has a strong predictive value for diabetes complications especially the microvascular complications (neuropathy, nephropathy and retinopathy). Studies showed that HbA1c reduction will result in fewer risk of microvascular complications in the immediate short term and macrovascular complications (cerebrovascular, cardiovascular, peripheral vascular) in long term. HbA1c level should targeted below 6.5% and more aggressive maneuvers should be initiated especially to those with long life expectancy and no comorbidities. In short, everyone with Diabetes Mellitus Type 2 should get their HbA1c level controlled to prevent further debilitating conditions. Healthy lifestyle, proper diet, compliance to medications are all the factors attributable to HbA1c level. I bet many of you have seen people with complications of Diabetes Mellitus such as Stroke, Heart Attack and amputated foot.
The government has spent billions to help these people to experience the best quality of life but you can guess how suffering will it be when you lose the ability to do your daily activities such as walking, going to the loo and etc. My mother has uncontrolled Diabetes Mellitus for many years and she experienced stroke few months ago, and it took a toll to her quality of life and even to us, her family members. We had to mobilize her from her wheelchair everywhere such as to the bathroom or to the sofa as she was unable to do it by herself. She was pretty much depressed about the whole situation which saddens the whole family too. Prevention is better than cure , so before all these tragedies occur, get your lifestyle right ! Thank you :)
References
- Clinical Practical Guidelines. Management of Type 2 Diabetes Mellitus. Fifth Edition. Malaysia: Malaysian Endocrine & Metabolic Society, 2015. Print
- Estimation of Blood Glucose Control in Diabetes Mellitus. UpToDate. Retrieved on May 1, 2018, from https://www.uptodate.com/contents/estimation-of-blood-glucose-control-in-diabetes-mellitus
- Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabete Mellitus. Abbreviated Report of a WHO consultation. World Health Organization. PDF file
- Analysis of HbA1c on Ion Exchange HPLC. Canterbury Scientific. Retrieved on May 1, 2018, from http://www.canterburyscientific.com/products/technical-information/hba1c-on-ion-exchange-hplc/
- What is HbA1c?. Diabetes info NZ. Retrieved on May 1, 2018, from http://www.diabetesinfo.org.nz/hba1c.html
- English E., John G. HbA1c (glycated hemoglobin) (blood). Association for Clinical Biochemistry 2012. PDF file.
- Ion Chromatography. Wikipedia. Retrieved on May 1, 2018, from https://en.wikipedia.org/wiki/Ion_chromatography


Very informative!
Hemoglobin is one heck of a molecule and its key role Physiology is what makes it very very interesting.
I expected to read something brief about the dissociation curve of the Oxygen or a brief comparation with the other types of Hb, but your post is really complete regarding the glycosilation of the molecule and the function/uses.
You have earned a new follower! :D
Thank you for reading :) Yeah, hemoglobin is a huge topic and certainly there’s a lot more to cover if I want to talk about it. But I’ve decided to cover its correlation towards sugar control, hence i’ve omitted those parts. Thanks again 😬