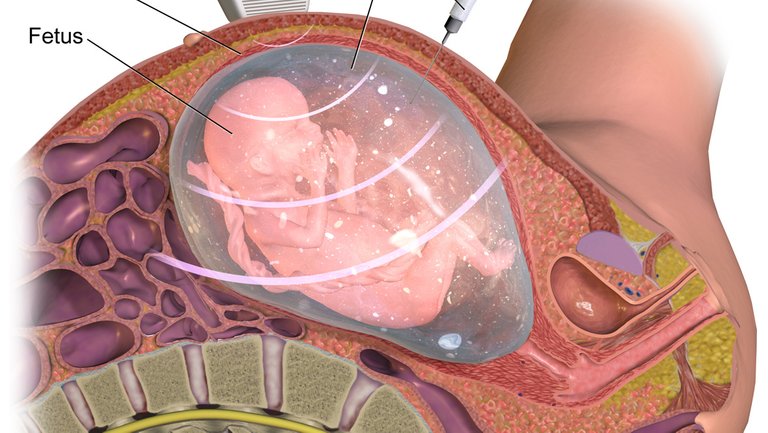
But some mammals like whales and dolphins are aquatic. How do they manage? They have learned to hold their breathe underwater and come up for air when necessary. But humans can 'breathe underwater.' Nature found a way through the placenta. The amniotic fluid is a liquid contained in a bag within which the fetus floats. Through this liquid medium exchange of nutrient with the mother occurs, and the fetus is cushioned and protected against physical shocks. The joy of motherhood. You know what they say about a baby’s first cry. A babe leaves the warmth and safety cocoon of the amniotic fluid and is suddenly thrust into the world. I would be angry too. A newborn child is so precious and their development 'pre' and postnatal fascinating. During this period, a lot of changes occur in the infant to prepare him for life in the outside. The difference between the physiology and anatomy of blood circulation and development in the 'pre' and postnatal life is so jarring that by the end of the post, we will all understand why every child must enter this world with a cry. Previously, we’ve looked at the cardiovascular system and the hemodynamics of blood flow. At the end of everything, the goal of fetal circulation and homeostasis is to ensure the supply of nutrient and oxygen to the developing tissues. To achieve this, the burgeoning fetal heart and blood vessels must overcome several limitations. In the intrauterine life, the lungs and liver are underdeveloped. Though by six months the lungs are fully developed, the infant can’t use it because he lives in a liquid environment. The child depends on the mother instead. The alveoli are collapsed, and the lungs are filled with fluid, so the first breath will be difficult. Two arms of the circulation nourish the growing fetus- its developing fetal circulation (made of the fetal heart and blood vessels) and the fetoplacental arm. The fetus is entirely dependent on the mother for nutrients and oxygen which are delivered to the fetus through the placenta and umbilical cord. The placenta is an organ linking the fetus to the uterine wall and facilitating nutrient uptake, temperature regulation, immune system development and waste elimination for the growing infant. To put this in perspective, the mother helps the fetus to ‘eat,’ ‘respire,’ ‘excrete’ and grow. It is little wonder why mothers have the maternal ‘lioness protecting her cub’ instincts. Blood circulation in the fetus differs from the usual for several reasons. The fetal heart has the natural right and left heart with its four chambers, the right ventricle, left ventricle, right atrium and left atrium. But the fetal lung and liver are underdeveloped. Of vital importance is the underdeveloped lung because pulmonary oxygenation of blood cannot occur. The mother delivers oxygenated blood to the growing infant through its connection to the placenta. The fetus is connected to the placenta through the umbilical cord. Due to the inability of the underdeveloped lung to oxygenate the blood, there is virtually no need for the pulmonary circulation. Yet if the muscles of the right heart (the pulmonary circulation) aren’t used adjustment to postnatal life would be impossible. What a dilemma. The fetal heart overcomes this by creating three shunts diverting blood away from the lung. A shunt is any direction of blood flow that doesn’t follow the usual route. Normal blood flow in the heart follows the right atrium→right ventricle→lungs→left atrium→left ventricle. Shunts direct blood flow away from this pattern. The aim of these shunts is not only to bypass underdeveloped organs but to ensure blood supply to the fetal brain is never undermined. Note that regardless of the relationship between mother and child (the placenta), blood from the mother NEVER mix with fetal blood. The three shunts in the fetal circulation Recall that these shunts exist to bypass underdeveloped organs. The ductus venosus shunt helps the fetal circulation bypass the liver by linking the left umbilical vein to the inferior vena cava. But the developing liver is kept nourished as a part of the blood supply through the umbilical vein goes through the left portal vein then back to the ductus venosus and the inferior vena cava. The foramen ovale is a cardiac right to left shunt in the interatrial septum that helps to divert blood from the right atrium to the left atrium. The foramen ovale is formed during the fourth week. It is one of the two cardiac shunts as the ductus venosus is located outside the fetal heart. This shunt links the fetal pulmonary artery to the descending aorta, mediating the diversion of blood away from the developing lungs. Since the developing fetus lives in an ‘aquatic’ environment inside the amniotic cavity, as explained in the first paragraph, breathing would be impossible, so the lungs are unnecessary. Therefore, the fetus depends on the mother for oxygen. Even as the fetoplacental circulation helps to keep the fetus alive by delivering oxygen, the underdeveloped lungs continue to grow. Oxygenated blood from the placenta travels within the umbilical vein. A branch of the umbilical vein goes to supply the liver directly. Another part enters the inferior vena cava through the ductus venosus to be emptied into the right atrium. Another branch links to the portal vein and back to the right atrium. Usually, from the right atrium, the blood moves to the right ventricles to the pulmonary artery to the lungs. But to bypass the underdeveloped lungs, the fetal blood passes to the left atrium through the foramen ovale. From the left atrium, the blood moves to the left ventricle where it is pumped into the aorta. The coronary circulation is supplied with oxygenation blood then the oxygen-poor deoxygenated blood is dumped into the right atrium. Deoxygenated blood from the superior vena cava is also delivered to the right atrium, so there’s a mixing of deoxygenated and oxygenated blood in fetal circulation. The fetal hemoglobin is different from the adult hemoglobin. Fetal hemoglobin has a higher affinity for oxygen than adult hemoglobin. This important property helps the fetal blood ‘steal’ a lot of oxygen from the mother. This affinity for oxygen also helps to overcome the effect of deoxygenated blood mixing with oxygenated blood and allows the developing issues access to a lot more oxygen. It is the fetal blood pressure and not the mother’s that powers blood flow through its heart. Even though the lungs are underdeveloped, a small amount of blood passes through the right atrium, to the right ventricle to be pumped into the pulmonary circulation. But the ductus arteriosus linking the pulmonary artery to the descending aorta ensures the blood is diverted from the lungs to the aorta. When the umbilical cord is cut, the child can no longer depend on the mother. Immediately the baby is born and takes that first, difficult breath using its own lungs, several changes occur. With that first breath, the collapsed lung begin to expand, and the pressure in the pulmonary circulation decreases. The fluid-filled lungs are slowly drained of fluid, and the child’s blood pressure begins to rise, prompting the ductus arteriosus to close. The increased pressure in the systemic circulation over the pulmonary whose pressure increases with the first breath causes the foramen ovale to close. The movement of oxygen-rich blood through the ductus arteriosus also causes secretion of baradykinin that mediates smooth muscles contraction and closure of the ductus arteriousus. After the closure of these shunts, a small ligament remains. These are- When these shunts fail to close, they result in severe, fatal pathophysiologies. Each ‘un-closed’ shunt is named by adding ‘patent’ to its name. In patent ductus arteriosus the ductus arteriosus remains open allowing blood from the aorta go back to the lungs. When the infant makes the first cry and breathes, the pulmonary vascular resistance decreases while the systemic vascular resistance increases. As a result, the left atrium now has a higher pressure than the right, causing a back flow of blood through the ductus arteriosus into the pulmonary artery. The pulmonary artery delivers this ‘backflow’ blood to the lungs to be re-delivered to the left atrium and back again. This causes the cardiac output to increase abnormally and can lead to pulmonary congestion. Patent ductus venosus occurs when the ductus venosus remain open. A persistent ductus venosus after birth can lead to liver failure, pathophysiologies of decreased liver function and jaundice later because the ‘bypassed’ liver won’t be adequately perfused. Patent foramen ovale is an atrial septal defect where the foramen ovale shunt linking the right atrium to left atrium fails to close. In some persons, it doesn’t completely close and raises no complications. But in many cases, it can be fatal as some of the oxygenated blood in the left heart mixes with those in the right heart. The reduced pulmonary resistance and the lack of blood supply through the umbilical veins cause the systemic vascular resistance to increase. This increase in pressure in the left heart causes a backflow of blood through the patent foramen ovale to the right atrium, mixing oxygenated blood with deoxygenated blood that is then pumped through the pulmonary circulation to be oxygenated again. A patent foramen ovale is common and causes no complication unless another heart defect is present. Agpar test is a test administered to babies one minutes and five minutes post birth. On a scale of one to ten, the baby's color, respiratory reflexes, and muscle tone are observed and quantified. A score between four and six means the baby needs to be monitored while a score below four indicates the infant's life could be in danger. The Agpar test shows how well the baby is adjusting to postnatal life After birth, the infant is no longer dependent on the mother for nutrients through the placenta. That baby's first cry expands the lungs and helps drain the amniotic fluid from the airways and lungs. The pulmonary resistance is lifted, and the pulmonary resistance is reduced. The first independent breath marks the beginning of postnatal life. As the infant roars his disapproval, a smile will light up the mother's face. Amniotic fluid
Photo by freestocks.org from Pexels
Source:
A fetus suspended within the amniotic sac
The aim of fetal circulation

Prenatal life
The fetal heart starts beating by the fourth week following fertilization. The developing heart beats at the rate of 65beats/minute, and this value can increase to as high as 140 beats/minute just before birth.Placenta
For this post, we are concerned with what happens within the fetal circulation. Perhaps I would address fetoplacental circulation in another post.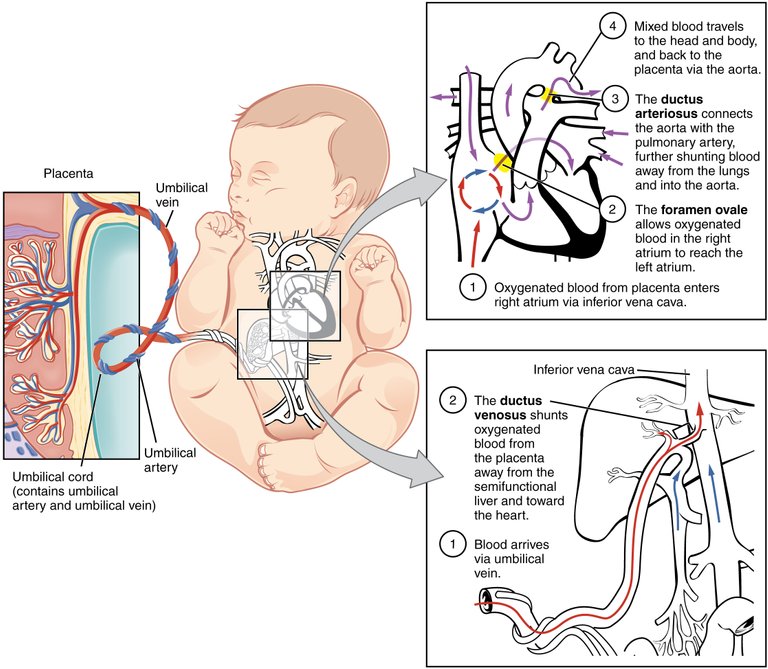 By: OpenStax College. CC BY 3.0
By: OpenStax College. CC BY 3.0
Source: Anatomy and Physiology connexions website, via Wikimedia Commons
Foramen Ovale
Ductus arteriosis
Fetal lungs
Blood from the aorta enters the internal iliac arteries then to the umbilical arteries which carry deoxygenated blood to the placenta where the wastes are dumped.
Due to the underdeveloped nature of the lungs, vascular resistance in the pulmonary circulation in the fetus is high while systemic vascular resistance is low, allowing blood to flow freely through the blood vessels.'Muscle Memory' in the fetal heart
You can see that even with the presence of the shunts, a small amount of blood is still supplied to the ‘bypassed’ organs. This is to keep them alive (liver and lungs) and ensure the muscles are ready for postnatal life. (the right heart)
As the pressure in the right atrium decrease, the systemic vascular resistance and pressure in the left atrium to rise, it prompts the foramen ovale to close also. These shunts should be closed off for the child to survive postnatal life. In some people, the foramen ovale don’t completely close off and usually don’t constitute a problem.
At birth, these changes occur to mediate a smooth transition to postnatal life.
Research has shown that prostaglandin E2 (PGE2) and prostaglandin I2 (PGI2) play a role in ensuring patency of the ductus arteriosus. But at birth, an increase in oxygen concentration and a decrease in the prostaglandin E2 (PGE2) and prostaglandin I2 (PGI2) causes the ductus arteriosus to close.
When the umbilical cord is severed, blood supply to the child through the umbilical veins ceases, this cessation and increase in systematic blood pressure causes the ductus venosus to close. Also, the decreased pressure in the portal vein kick-start the closure within minutes of postnatal life. The closure is completed over the next three to seven days.Remnant of shunts
- shunt remnant 1 Ductus venosus Ligamentum venosum 2 Ductus arteriosus Ligament arteriosum 3 Foramen ovale fossa ovalis
Welcome to a new world.
Blood circulation in the fetus and newborn
Blood circulation in the fetus and newborn
Cardiac shunts
Fetal circulation
Fundamentals of environmental measurements
Fetal circulation: Anatomy and Physiology
Fetal hemoglobin
Ductus venosus
Guyton, Arthur C, and John Hall, Textbook of Medical Physiology. Elsevier, 2000.
Phases of lung development
Patent Ductus ateriosus
Why can’t human beings breathe
underwater?
Placenta
Prostaglandin E1 for maintaining ductal patency in neonates with ductus-dependent cardiac lesions
First cry of newborn

Fetal Circulation
Why can’t humans breathe underwater? One of my favorite song is Breathing Underwater by Metric. (I’m an alternative rock addict.)
The question above seems like a strange one. Naturally, we can’t breathe underwater for several reasons. One, we do not have gills, the specialized respiratory organ with a large surface area that helps many aquatic organisms extract dissolved oxygen from water. Two, we are warm-blooded animals with a higher need for oxygen than the concentration of dissolved oxygen present in water bodies. Dissolved oxygen is free unbound oxygen present in water bodies that are necessary for the survival of aquatic life. Humans need far more oxygen than that. Furthermore, our lungs are not designed to extract oxygen from water as gills are.
By: BruceBlaus, CC BY-SA 4.0
Wow. That is piece of a great work.
It also does look so much nicer when text is justified. Obviously upvoted.
ps. wouldnt it be cool if humans could breathe under water? but wouldnt we destroy entire planet earth if we could?
yes, it does look better. Thanks
How incredible.
Almost unbelievable evolution led to such complexity and incredible design.
Nature is amazing.
Yes. It's awe inspiring.
I like how you wrote this as a story, not just facts, @vanessahampton. Are you a med student?
It is truly incredible how all development is coordinated. Life is magnificent!
P.s. it's Apgar test ;)
Thanks, i always misspell and mispronounced it all the time. Thanks for noticing that. Yh, life is...everything.
Funny enough, this is what we are being taught under embryology, starting from fertilization to implantation, the corpus luteum, 1st week of embryonic life, gastrulation, growing of the fetus, the germinal layers. When I saw this post, I was like wow, more education. Thanks.
Thank u too